Types of cervical cancer
Cervical cancer varies because the cells in which the cancer starts differ. Although there are different types of cervical cancer, the most common types include the following.
Squamous cell cancer
It is a type of cervical cancer that starts in squamous cells, which are thin and flat cells. These cells are located on the outside of the cervix. Squamous cell carcinoma is the most common type of cervical cancer.
Adenocarcinoma
The column-shaped cells are called adenomas. The type of cervical cancer that starts in these cells in the cervical canal is called adenocarcinoma.
In some cases, it is seen that both types of cancer start at the same time. Other types of cells in the cervix can also develop cervical cancer. However, this is a very rare situation.
Symptoms of Cervical Cancer
Cervical cancer usually takes years to decades to develop from tissue changes. They are usually harmless and cause little or no discomfort. Once cancer has developed, it can manifest itself with the following symptoms:
- Unusual bleeding: for example after sexual intercourse, outside menstruation or after the last menstrual period during menopause
- unusual, sometimes foul-smelling, vaginal discharge
- fatigue and weight loss
- abdominal and pelvic pain
- pain when urinating
When cervical cancer causes symptoms, it is usually already advanced.
Causes of Cervical Cancer
The main cause of cervical cancer is the human papillomavirus. This family of viruses, also called HPV, causes cervical cancer. Among the areas where HPV types can be transmitted are the following.
- Skin-to-skin contact of the genital area
- Sharing sex toys
- Vaginal, oral or anal sex
In addition, some groups have a higher risk of developing uterine cancer. The characteristics of this group include the following.
- Women under 45 years of age
- Having a weakened immune system
- HIV or AIDS patients
- Giving birth to more than one child
- Having children under 17 years of age
- Previous bladder, vulval, kidney or vaginal cancer
- Smoking and using tobacco products
- High number of sexual partners
- Early sexual activity
- Other sexually transmitted infections
- Exposure to anti-abortion drugs
Risk Factors for Cervical Cancer
Some women are more likely to develop cervical cancer than others. This applies, for example, to smokers, probably because their immune system fights the virus less effectively. Diseases such as AIDS or medications taken after organ transplants weaken the immune system and make people more susceptible to HPV infections.
Because HPV is sexually transmitted, generally all factors and behaviors that increase the risk of sexually transmitted infections are also considered risk factors for cervical cancer. For example, the risk increases with the number of sexual partners.
Incidence of Cervical Cancer
Approximately 4,600 women in Turkey develop cervical cancer every year. About 1600 women die from it. The risk of cervical cancer depends mainly on whether a woman has been screened, whether she has been vaccinated against HPV and how old she is.
How is Cervical Cancer Diagnosed?
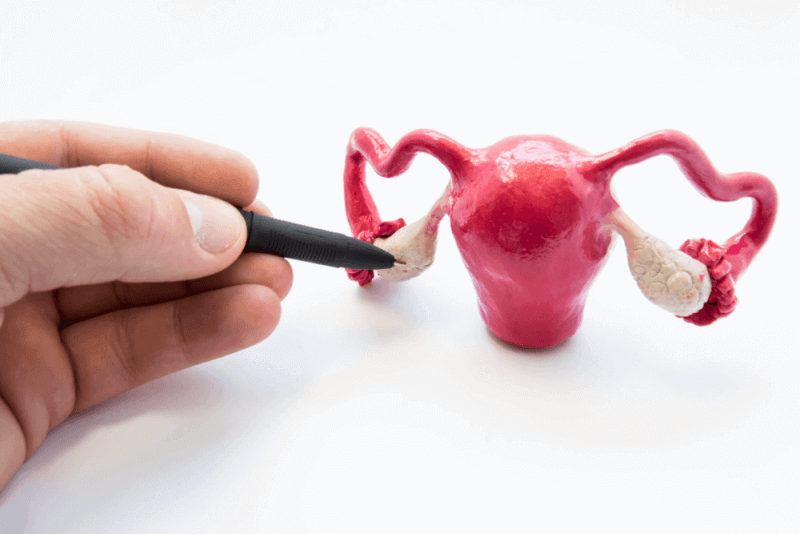
Precancerous lesions or suspicion of cervical cancer can be indicated by symptoms, a PAP smear test or gynecological examination is often helpful. During the examination, the gynecologist feels the uterus on the abdominal wall and vagina. He also inserts an instrument (speculum) into the vagina to look at the tissue around the cervix. If the changes are more severe, the tissue in the cervix can be examined with a kind of magnifying glass (colposcopy). A tissue sample may also be taken (biopsy). This is examined in a laboratory.
If a pre-stage or suspicion of cancer is confirmed, the next procedure depends on how advanced the tissue changes are. Small changes or tumors can be removed surgically.
Ultrasound, X-rays, magnetic resonance imaging or computed tomography are necessary if the cancer has spread to deeper layers of tissue. In addition, a laparoscopy is often performed to remove the lymph nodes. Based on these examinations it is possible to assess how far the cancer has progressed.
Early Diagnosis
Early stages of cervical cancer can be detected and removed with screening tests, potentially before it develops into cervical cancer. For this purpose, a cell smear examination is performed. A PAP smear test can be used. It is very important that the doctor performing this test is experienced. Since the introduction of regular examinations in the 1970s, significantly fewer cervical cancers have developed than in previous decades.
Women between 20 and 34 years of age can get tested once a year. A swab is taken from the cervix and examined in the laboratory. Women over 35 can opt for a combined examination every three years. Be aware of the importance of early detection and get tested regularly. Spread is examined both in terms of HP viruses and cell changes.
Further tests can be performed according to the results of early diagnostic examinations.
Cervical cancer test
Cervical cancer tests are performed both at diagnosis and during follow-up examinations for prevention. With the help of so-called screening tests, cancer can be detected in the early stages. Diagnostic tests are more comprehensive and are used not only for diagnostic purposes but also for important points such as cancer staging.
Cervical cancer screening
These tests are performed without any symptoms and usually during routine gynecology examinations.
HPV test
Since the human papillomavirus is the primary cause of cervical cancer, it is a priority in screening tests. With this test, it is possible to test people for infections caused by HPV types.
PAP SMEAR test
This test, in which various cells are collected from the cervix, screens for cells that could develop into cervical cancer if left untreated. It enables early detection of cell changes caused by HPV. This test is used not only to detect cancer cells but also to detect non-cancerous conditions such as infection and inflammation.
HPV/ PAP cotest
It is a test that checks for both high-risk HPV and changes in cervical cells. This test uses HPV and the PAP SMEAR test together.
Diagnostic tests
Cervical cancer can be treated by using different tests if symptoms of cervical cancer are observed or if suspicion is found during routine checks. These tests are extremely important not only in the diagnosis of cervical cancer but also in the planning of treatment.
Bimanual pelvic examination and sterile speculum examination
In this examination, which can also be called gynecological examination, the gynecologist and obstetrician checks whether there are any changes in the cervix, uterine entrance, ovaries, vagina and other nearby organs.
For this, the vulva is first examined and checked for any changes. Then, with the help of an instrument called a speculum, the vaginal walls are kept open so that the inside of the vagina can be seen. A PAP SMEAR test is also performed at this stage.
However, it is not possible to see nearby organs at this stage. For this reason, the doctor performs a palpation and applies gentle pressure to the lower abdomen. This examination, which usually takes a few minutes, is performed under clinical conditions.
Colposcopy
Colposcopy, which enables the detection of abnormal areas in the cervix, is also a method used to guide cervical biopsy. During the colposcopy procedure, an instrument called a colposcope is used, which allows the cervical cells to be seen like a microscope.
The colposcopy examination is similar to the speculum examination. For this reason, it is a procedure that can be applied in the doctor's office. Colposcopy, which is a safe method, is also a test method that can be applied to women during pregnancy.
Colposcopy is recommended for people with suspicious or positive results in cervical cancer screening or ASCO screening.
Biopsy
A positive biopsy result is essential to confirm the diagnosis of uterine cancer. Tissue samples taken from the cervix should be examined under a microscope. Afterwards, the pathologist must evaluate the results and cell values and reach a conclusion. There are different types of biopsy.
Cervical curettage (ECC)
ECC is used to check areas not seen during colposcopy. For this procedure, a small amount of tissue is scraped from the opening of the cervix. A spoon-shaped instrument called a curette is used for this procedure.
Loop electro surgical excision procedure (LEEP)
This test, in which an electric current through a thin wire hook is used to harvest tissue, makes it possible to harvest tissue for examination in the laboratory. LEEP can be used for diagnosis as well as for the treatment of precancerous or early stage cancer.
Conization (cone biopsy)
In the conization procedure, which can be performed under general or local anesthesia, the tissue taken in the cervix area is cone-shaped. It is a procedure that can be performed under both operating room and clinic conditions and can also be used for the treatment of early stage cervical cancer.
Pelvic examination under anesthesia
Pelvic examination under anesthesia is a technique used in the planning of treatment. While the patients are under anesthesia, a detailed examination of the pelvic area is performed. This can help determine whether the cancer has spread to nearby organs.
X-ray
It is used to visualize the kidneys and bladder and to determine whether cancer has spread to these areas.
Computed tomography
Computed tomography is used to detect any abnormalities in the structures or the presence of tumors. It is also used to measure the size of the tumor. In some cases, a contrast agent is administered to obtain a more detailed image. The contrast medium can be administered intravenously or in pill form.
Magnetic resonance imaging
It is an imaging method that uses magnetic fields instead of radiation to visualize parts of the body. In this imaging method, which is used to measure the size of the tumor, a contrast agent can also be used to obtain a more detailed image.
Positron emission tomography (PET) or PET-CT scan
It is often combined with a CT scan, which doctors refer to as a PET scan. Before this scan, patients are given a small radioactive sugar load. This sugar is administered intravenously and absorbed by the cancer cells. Afterwards, the areas of the body where the radioactive region has accumulated are scanned. The areas where the substance accumulates are also cancer cells.
Tumor biomarker testing
It is a test to identify specific genes, proteins and other tumor-specific features. The results of the tumor marker test, also called the molecular test of the tumor, are effective in planning the treatment.
If patients have rectal or bladder symptoms, the following tests may be performed in addition to these tests and imaging methods. These procedures can be performed during a pelvic examination.
Cystoscopy
It is a procedure performed with a special instrument with a light and camera at the end to visualize the inside of the urethra. Patients can be sedated during the procedure. Cystoscopy is used to determine whether the cancer has spread to the bladder and urethra.
Sigmoidoscopy
It is a procedure performed with an instrument with a light and camera at the end that allows the colon and rectum to be examined. Patients are sedated before the procedure begins. It is used to determine whether the cancer has spread to the rectum and colon.
How to Prevent Cervical Cancer?
Cervical cancer almost always develops as a rare late diagnosis of infection with certain HPV viruses. Three ways of prevention are therefore - at least theoretically - possible:
- sexual abstinence or condom use
- Vaccination against the HPV virus
- Early detection and elimination of tissue changes
Anyone who wants to protect themselves from infection should abstain from sexual intercourse or only have intimate contact with someone with or without another sexual partner.
Condoms can provide effective protection against many sexually transmitted diseases and are therefore definitely useful if you have different sex partners. However, they do not provide reliable protection against HPV as they do not protect all areas of skin in the genital area that can be affected.
There are vaccines that can prevent cervical cancer. It is recommended that young people be vaccinated between the ages of 9 and 14, i.e. before first sexual contact. Boys and men can also be vaccinated. Even if they are infected later, they do not transmit HPV viruses.
How is Cervical Cancer Treated?
Which treatment makes sense depends primarily on how big the cervical cancer is and whether it has spread. If the tumor is very small, a small procedure on the cervix (conization) is sufficient. If the tumor has already spread to the surrounding tissue, doctors usually recommend surgery to remove the entire uterus (hysterectomy). In addition, the lymph nodes are extensively removed. Radiation is also an option. Radiation is also an option when a tumor can no longer be removed by surgery. In some patients, combined chemotherapy may also help. After cancer treatment, there is usually a right to rehabilitation (follow-up treatment).
The treatment is planned exactly for you. If the cancer has not spread to distant lymph nodes or organs, more than half of those affected can be treated. Specialists then recommend surgery or radiation chemotherapy.
The following surgical interventions may be considered:
- Konization Cutting part of the cervix. This may be sufficient treatment for very small and early detected tumors.
- Trachelectomy Partial removal of the cervix. The procedure is only considered if the cancer is very small and the lymph nodes are not affected. Pregnancy is still possible.
- Hysterectomy Removal of the uterus. Experts recommend this procedure when family planning is complete or when the cancer has already gone deeper into the tissue. This surgery may vary depending on how the cancer has spread.
In the case of advanced tumors or affected lymph nodes, experts recommend radiation chemotherapy. This is usually a comprehensive treatment. It is a better choice than surgery, which can be very stressful for the patient.
Cervical cancer vaccine
HPV, the main cause of cervical cancer, is a type of virus that is spread through sexual activity. This virus can also cause genital warts, while some strains can cause cervical cancer. Usually the immune system is able to clear HPV viruses. However, if these viruses remain in the body for a long time and are not cleared, cervical cancer can occur.
What does the HPV vaccine do?
The HPV vaccine also provides protection against many types of cervical cancer, especially genital warts. For this reason, it also provides protection against cancers of the vulva, vagina, anus and penis caused by HPV.
Vaccination is a safe way of building the body's immune system response. Therefore, if a vaccinated person is infected with HPV, the immune system clears the virus as soon as possible.
Who should be vaccinated against HPV and when?
The HPV vaccine approved by the FDA is a vaccine that can be administered to anyone over the age of 9. The Centers for Disease Control and Prevention recommends routine HPV vaccination for children aged 12 and 12 years. The most important point is that the HPV vaccine is administered before the start of active sexual life.
For people under 15 years of age, 2 doses of vaccination are sufficient. 6 or 12 months between doses is considered sufficient. For people between 15 and 26 years of age, 3 doses of vaccination are recommended. The interval between each dose is recommended to be 6 months. Until the age of 26, people who have not completed all their doses are strongly advised to complete their doses.
Who should not get the HPV vaccine?
Among the people who should not get HPV vaccine are the following.
- Pregnant women
- People who experienced an allergic reaction after the first dose of HPV
- People who are moderately or severely ill
Cervical cancer vaccine side effects
Many studies on the HPV vaccine have proven that the vaccine is safe. In addition, mild side effects may be observed. These side effects include the following.
- Pain at the injection site
- Swelling
- Redness
- Dizziness
- Fainting
- Headache
- Nausea
- Vomiting
- Fatigue
- Fatigue
In addition to these symptoms, the CDC and FDA continue to monitor HPV vaccines for serious and unexpected side effects.
Stages of cervical cancer
Cervical stages can be mixed. This is because the phases alone do not provide detailed information. Therefore, when planning treatment, not only the stage but also the grade and characteristics of the tumor are taken into account. Basically, there are 4 stages of cervical cancer. However, the stages are subdivided into various subgroups.
Phase 1
First stage cervical cancer is divided into two. However, each stage is diversified in its own way.
Phase 1A
At this stage there are very few cancerous cells and they can only be seen under a microscope. Therefore, there is no spread to nearby lymph nodes and distant tissues.
1A1 phase
Stage 1B is another stage in which the cancer area can only be seen under a microscope. At this stage, which is limited to 3 mm in depth, there is no spread to nearby lymph nodes or distant organs.
1A2 phase
At this stage, the cancer site can only be seen under a microscope. However, its depth varies between 3 and 5 mm. It has not spread to nearby lymph nodes or distant organs.
Phase 1B
Stage B, the second stage of the first stage of cervical cancer, is divided into 3 subgroups. At this stage, the cancer cells are still confined to the cervix, but their depth is reduced to 5 mm.
1B1 phase
At this stage, it varies between 5 mm and 2 cm depending on the stage of cancer. It does not spread to nearby lymph nodes and distant organs.
1B2 phase
At this stage, the size of the tumor is larger than 2 cm and smaller than 4 cm. It does not spread to nearby lymph nodes and distant organs.
1B3 phase
At this stage, the tumor is larger than 4 cm. However, it is still seen in the cervix. Therefore, it has not spread to nearby lymph nodes and distant organs.
Phase 2
In the second stage of cervical cancer, there are no metastases in nearby lymph nodes or distant organs. However, the tumor has grown beyond the uterus. At this stage, the tumor has spread beyond the cervix, but not to the pelvic wall or the lower part of the vagina.
Phase 2A
Although tumor tissue can be seen beyond the cervix, it is not seen in the tissues called parametria next to the cervix. There is also no metastasis to nearby lymph nodes or distant organs.
2A1 phase
At this stage the tumor is no larger than 4 cm. There is no metastasis to nearby lymph nodes or distant organs.
2A2 phase
At this stage, the cancer is larger than 4 cm, but there is no metastasis to nearby lymph nodes or distant organs.
2B phase
At this stage, the tumor cells have grown beyond the uterus. This is why parametria propagation is observed. However, even at this stage, it does not spread to nearby lymph nodes and distant organs.
Phase 3
In the third stage of uterine cancer, cancer cells spread to the lower part of the vagina and the pelvic wall. Therefore, there is a possibility that the tumor may block the ureters at this stage. At this stage, cancerous tissue can also be found in nearby lymph nodes. However, metastasis to distant organs is not seen.
Phase 3A
At this stage, the cancer is visible in the lower part of the vagina but has not yet reached the pelvic wall. There is no metastasis to nearby lymph nodes or distant sites.
3D phase
In stage B of the third stage of the cervix, the cancerous tissue grows relative to the pelvic wall. For this reason, it can block one or both urethras. This leads to a health problem called hydronephrosis, which causes kidney problems due to blockage of the urethra. At this stage, metastases in nearby lymph nodes and distant organs are not seen.
3C phase
The tumor at this stage can be of any size. Imaging or biopsy shows spread to nearby pelvic lymph nodes or para-aortic lymph nodes. Metastasis to distant organs is still not seen.
Phase 4
Stage four, the last stage of cervical cancer, is also divided into two stages. At this stage, cancer starts to appear in organs such as the bladder, rectum, lung or bone.
Phase 4A
In the first stage of stage four, tumor cells spread into the bladder or rectum or begin to grow outward from the pelvis
Phase 4B
In stage 4B, the last stage of cervical cancer, cancer cells spread to distant lymph nodes, lungs and bones.
Can cervical cancer kill?
Cervical cancer, which is usually seen in women between the ages of 30 and 50 and who have an active sexual life, has an extremely high success rate in case of early diagnosis. However, in terms of mortality rates, cervical cancer still ranks high among the cancer types with the highest mortality rate.
Cervical cancer and sexuality
Cervical cancer is one of the types of cancer that affects women's sexual life. Although it is not yet known exactly how much cervical cancer affects the sexual life of patients, studies in this field are ongoing.
It is known that symptoms such as hair loss and fatigue, which are among the side effects of radiotherapy and chemotherapy used in the treatment of cervical cancer, affect the sexual lives of cancer patients. A significant number of experts believe that patients' sex lives are negatively affected even after treatment.
In particular, stigmatization and discrimination of patients cause a significant impact on their social lives. This leads to patients experiencing less sexual pleasure and being closer to psychological stress, which affects their sexual life.
Scientific studies in this field show that a significant proportion of patients have sexual dysfunction. In addition, multiple urine leakage also affects a significant proportion of patients. Other complaints reported by patients during cervical cancer treatment include the following.
- Loss of libido
- Vaginal dryness
- Pain during sexual intercourse
- Fatigue
- Agri
- Impaired sleep and rest
- Fertility problems
- Functional immobility
After the successful treatment of uterine cancer, the following are among the complaints seen in patients.
- Changing sex life
- Vaginal stenosis
These changes that patients experience after treatment may be associated with depression. For this reason, it is known that the quality of life of patients with sexual dysfunction is lower than those who maintain a normal sexual life.
Low libido
Both during and after treatment for cervical cancer, patients experience sexual reluctance and loss of desire. This is thought to be due to the fear of getting cancer and the side effects of treatment.
It may take some time for patients to return to their normal sex life. For this reason, patients are advised to have an open attitude towards their partners and to prefer methods such as cuddling and massage for intimacy.
Vaginal changes
If the ovaries are affected by radiation therapy for cervical cancer, estrogen production stops. This causes the vagina to dry out. Vaginal dryness causes the vagina not to expand easily during sexual intercourse. In addition, the lack of estrogen secretion causes the vagina to lose its elasticity and narrow.
The vaginal narrowing experienced by patients is also called vaginal stenosis. This change makes sexual intercourse difficult and can prevent orgasm. To overcome this problem, various methods and exercises should be used.
When can sexual life be resumed?
Being diagnosed with cervical cancer increases the risk of the HPV virus, causing patients to feel discouraged from sexuality or to experience anxiety about having sexual intercourse. But cervical cancer is not contagious. Therefore, it cannot be transmitted to the partner.
She can also have sexual intercourse during treatment. However, it is recommended that partners use condoms during this process. Although it has not yet been proven whether the HPV virus is transmitted through vaginal mucus, condom use is recommended as a precaution. There is also no definitive information on whether the medicines used in treatment can be passed on to the partner. This is why partners need to take precautions.
Experts recommend the end of treatment for people diagnosed with cervical cancer to resume their sexual life. Patients need several weeks of rest to complete the radiotherapy sessions and for the tissues to recover after the surgery. They can then return to their sexual life. Having an active sex life does not cause the cancer to recur or worsen.
Can cervical cancer kill?
Detailed studies have been conducted on the 5-year survival rates of patients after treatment of cervical cancer. According to these studies, survival rates according to the diagnosed stages of cervical cancer are as follows.
- The 5-year survival rate of cervical cancer patients diagnosed at an early stage is 91%.
- If cervical cancer spreads to nearby tissues and organs or metastasizes to regional lymph nodes, the 5-year survival rate is 60%.
- If the cervix metastasizes to distant tissues and organs, the 5-year survival rate of patients is 519.
- On average, the 5-year survival rate of cervical cancer patients is 67%.