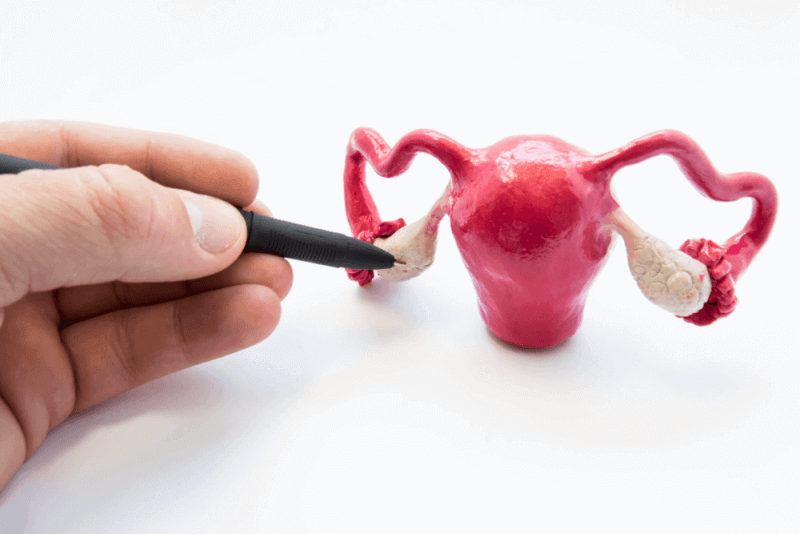
What is Cervical Failure?
|
In case of cervical insufficiency 2. During pregnancy in the trimester, there is recurrent painless dilation of the cervix (cervix uteri) without contractions. There is a simultaneous dilation and softening of the cervix and a shortening of the cervix to less than 2.5 cm. If it goes unnoticed, cervical insufficiency can lead to pregnancy loss. |
Doctors speak of cervical insufficiency when the cervix and cervical canal are softer and shorter than normal. A weak cervix usually does not affect women's lives. However, in pregnancy, cervical insufficiency increases the risk of premature birth. This is especially true for the average third of pregnancy. The main causes of weakening of the cervix and cervix are weaknesses in the connective tissue, childbirth (especially multiple births), surgery and infections.
Causes of Cervical Failure
A multifactorial genesis is suspected, involving infections as well as immunologic and mechanical causes. Increased infections with beta-hemolytic streptococci, chlamydia, ureaplasma, gardnerella or other microbes play an important role here. They are important because of the release of inflammatory mediators (e.g. prostaglandins) associated with infection.
Pure istmoscervical insufficiency is rare today. In the past, it was predominantly observed after abortion. Mechanical trauma to the cervix caused damage to the cervical closure mechanism. The possibility of early medical termination of pregnancy and the use of prostaglandins to dilate the cervix have contributed to the fact that isthmoscervical insufficiency is almost never observed.
The exact causes of cervical insufficiency are unknown. It is now assumed that hormonal changes play an important role in an average of one third of pregnancy (2nd trimester). Apparently, hormonal changes cause premature softening of the tight connective tissue of the cervix and cervical canal. This tendency appears to be inherited. In addition, the cervical canal in women is sometimes shorter than 2.5 cm. This is also considered a risk factor for cervical insufficiency. Other risk factors include uterine abnormalities, excessive amniotic fluid, previous pregnancy and birth (especially multiple births), and infection or surgery of the birth canal and uterus.
Pathophysiology
It is triggered by increased intrauterine pressure (IUD) encountering a structurally weakened cervix. There is early disintegration of the cervical collagen structure. As a result, the cervix can no longer cope with the increased pressure and dilates.
Risk Factor for Cervical Failure
There is an increased risk after previous surgical interventions such as conization and after mechanical cervical dilatation in the context of gynecological interventions. Injury to the cervix uteri in previous pregnancies and congenital uterine anomalies can also cause cervical insufficiency.
Another risk factor is multiple pregnancies.
Symptoms of Cervical Failure
Patients with cervical insufficiency in the current pregnancy are mostly asymptomatic. It may include mild symptoms such as
- pressure in the pelvis or vagina
- menstrual-like cramps and/or back pain
- changes in vaginal discharge
Symptoms usually appear in the 14th week of pregnancy. and 20. It starts between weeks.
A weak cervix is not necessarily noticeable with obvious symptoms during pregnancy. Sometimes cervical insufficiency is diagnosed only after one or more miscarriages.
Menstrual-like symptoms may indicate a weak cervix. Pulling or pressure in the pubic bone, lower back or groin area are also possible symptoms of cervical insufficiency. Premature rupture of the canal without contraction, bleeding and prolapse of the amniotic sac into the vagina are strong signs of cervical insufficiency.
If you have symptoms - especially in the average third of pregnancy - you should urgently talk to your gynecologist.
Pregnant women with an incompetent cervix usually experience mild symptoms in the second trimester between 14 and 20 weeks. Women who have not had a miscarriage due to cervical insufficiency can sometimes miss these subtle symptoms. It is very important to talk to your doctor immediately if you experience any of the following symptoms
- spots or light bleeding from the vagina
- feeling of pressure in the pelvic area
- cramping pain in the uterus
- back pain
- a clear white discharge from the vagina that turns pink over time
During regular examinations, the doctor usually checks the length of the cervix and also cervical dilatation to rule out a case of insufficiency.
Complications of Cervical Failure
Without timely treatment, a woman with an incompetent cervix can face many complications during pregnancy, such as
- Premature Birth - If the cervix opens later in the second trimester, there is a possibility that the baby will be born prematurely. In this case, the baby will need life support and an incubator until it reaches a stage where it can function independently.
- Stillbirth - The 20th day of pregnancy when a pregnancy is called stillbirth. Pregnancy loss occurring after the first week of pregnancy. If the baby is born too young, it often does not have the growth and development to survive outside the womb.
- Miscarriage - Babies born to mothers whose cervix weakens between 18 and 22 weeks often miscarry. A fetus cannot survive if it is born before 23 weeks.
While these complications are ongoing, timely corrective measures such as medications, surgery and rest periods can help many mothers successfully deliver all their babies.
How is Cervical Failure Diagnosed?
Diagnosis of cervical insufficiency is based on a typical obstetric history in combination with transvaginal ultrasound measurement of cervical length. A sonographic cervical length ≤ 25 mm before 34+0 weeks of gestation is considered shortened. In patients with advanced cervical dilatation, physical examination, inspection and palpation alone are sufficient to diagnose cervical insufficiency.
Contractions should be ruled out by tocodynamometry.
How is Cervical Failure Treated?
Treatment of cervical insufficiency depends on the cause and how acute the risk to the fetus is. In some cases, controlled preterm delivery is used. This is usually delayed as much as possible with the help of medication. Ideally, the lungs of the unborn child should be mature by the 34th week of pregnancy. premature labor should not be induced before the first week of pregnancy.
Sometimes natural birth is possible despite a weak cervix. To make this possible, the cervix can be closed with a cerclage (a type of rubber band). Sometimes the cervix is completely sutured before delivery.
Cerclage
Cerclage is used to stabilize the inadequate cervix in women with a preterm postpartum condition and a cervix length of less than 25 mm before 24+0 weeks of gestation. Prophylactic or elective cerclage is generally not indicated in the presence of risk factors or cerclage in a previous pregnancy. In appropriate cases, emergency cerclage can result in a valuable prolongation of pregnancy.
Non-surgical measures
Non-surgical measures include bed rest. For advanced cervical changes, it is probably used in combination with antibiotics and indomethacin administration. It is also possible to use pessaries that change the axis of the cervical canal according to the vaginal axis.
Progesterone supplementation:
Progesterone is a natural steroid hormone administered in the second trimester to prevent miscarriage and premature birth. It is usually given weekly or as preparations that can be inserted through the vagina. However, this treatment option is not successful in including multiple pregnancies.
Continuous monitoring:
In women with an incompetent cervix or a damaged cervix in the past, doctors usually use ultrasound to measure the length of the cervix every two weeks. If the cervix opens during this continuous assessment, the doctor immediately performs an operation called cervical cerclage to sew the opening in the cervix.