What is diabetic retinopathy?
Diabetic retinopathy is an eye disease that affects the retina. All people with diabetes can develop this condition. If left untreated, diabetes-related retinopathy can lead to vision loss.
Diabetic retinopathy diagnosis
Diabetes-related retinopathy can be diagnosed with a simple examination. Among the tests performed during the examination are the following.
- Sight acuity test
- Intraocular pressure to make sure there are no signs of glaucoma;
- Eye muscle function
- Environmental opinion
- Response to light
Eye doctors put a special drop in the eye during the examination. This dilates the pupils and the doctor looks for the following criteria.
- Anomalous blood vessels
- Bleeding in the middle of the eye
- Growth of new blood vessels
- Retinal swelling
Causes of diabetic retinopathy
Over time, too much sugar in the blood can cause the small blood vessels that supply the retina to become blocked, cutting off the blood supply. To rule this out, new blood vessels begin to form in the eye. However, these new blood vessels do not develop properly and can easily leak without blood.
Symptoms of diabetic retinopathy
In the early stages of diabetic retinopathy, there may be no symptoms. Symptoms that can be seen as the disease progresses include the following.
- Floating spots or dark stripes in vision
- Cloudy vision
- Fluctuating vision
- Dark or empty areas in vision
- Loss of vision
- Color blindness
- Night blindness
- Problem reading or seeing distant objects
Diabetic retinopathy treatment methods
Various factors are taken into consideration when formulating treatment for diabetic retinopathy, including the following.
- Age
- Medical history
- The extent of retinal damage
- Visual acuity
- HgbA1c
In the early stages of the disease, specialists may use a wait-and-see approach, especially in cases of good vision. At this stage, regular eye examinations are performed. However, no further treatment is applied. Some patients need eye examinations every 2 to 4 months.
Diabetic retinopathy needle treatment
Medicines such as antivascular endothelial growth factor drugs or corticosteroids are injected into the eye. These injections slow the progression of the disease and improve vision. These drugs, called vascular endothermal growth factor inhibitors, are injected into the vitreous of the eye. This stops the growth of new blood vessels and reduces fluid build-up.
The procedure is performed using topical anesthesia. It may cause mild discomfort such as burning, tearing or pain for 24 hours after the injection. Possible side effects of the treatment include pressure build-up in the eye and infection. The injections require repeated treatments. In some cases they are used in combination with photocoagulation.
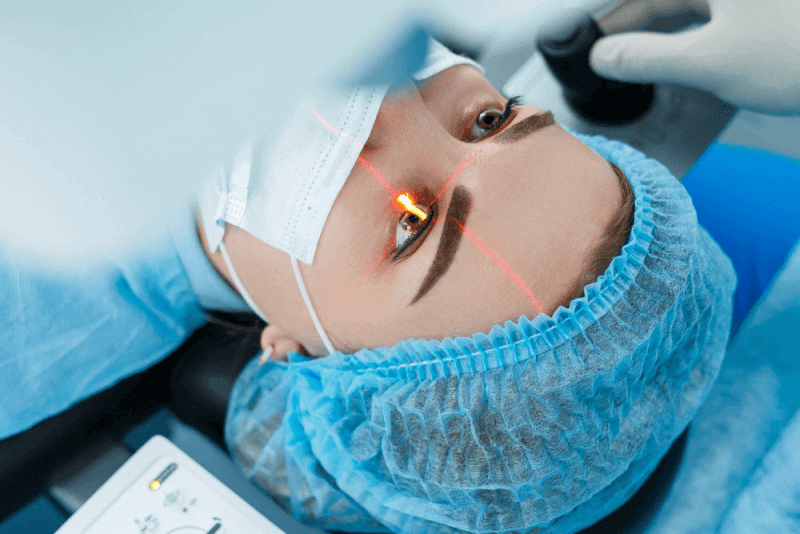
Diabetic retinopathy laser treatment
Laser surgery can be used to reduce swelling and new blood vessel formation in the retina. Laser treatment is divided into photocoagulation and panretinal photocoagulation.
Photocoagulation, also known as focal laser treatment, is used to stop or slow the leakage of blood and fluid from the eye. During the procedure, leaks from abnormal blood vessels are treated with laser burns. Focal laser treatment is usually performed in a single session in a doctor's office.
In patients with blurred vision due to macular edema before surgery, the treatment may not restore normal vision. However, it may reduce the likelihood of worsening macular edema. Panretinal photocoagulation is called scatter laser therapy. This treatment can shrink abnormal blood vessels.
Distributed laser burns are applied to areas of the retina away from the retina during the procedure. The burns upset the abnormal new blood vessels and cause scarring. It is usually performed in 2 or more sessions in the ophthalmologist's office or eye clinic. Patients' vision is blurred for one day after the procedure. Patients may also lose peripheral vision or night vision after the procedure.
Diabetic retinopathy surgery
This procedure, called vitrectomy, is performed through a small incision in the eye to remove scar tissue as well as blood from the center of the eye. It is a procedure that should be performed in a hospital using local or general anesthesia.
Methods of diabetic retinopathy surgery
Vitrectomy, an eye surgery procedure in which the vitreous fluid is removed from the eyeball, is also performed on diabetic retinopathy patients. In this procedure, the gel-like substance towards the center of the eyeball is removed. Various repairs are then made to the retina at the back of the eye.
After the necessary repairs are made, the viterus can be replaced with sterile saline, silicone or gas bubbles. This helps to maintain the shape of the eye and keep the retina in place. Vitrectomy is divided into two types: anterior vitrectomy and posterior pars plana vitrectomy. For diabetic retinopathy patients, posterior pars plana vitrectomy, which allows intervention in the back of the eye, is usually performed.
Benefits of diabetic retinopathy surgery
Vitrectomy is a procedure used to treat eye conditions that can cause vision loss and even blindness. It can also help the ophthalmologist make the correct diagnosis and provide better treatment.
Complications of diabetic retinopathy surgery
As with all surgical procedures, vitrectomy has some risks and complications. These complications include the following.
- Infection
- Bleeding
- Retinal tear
- Retinal detachment
- The development of a new cataract or faster growth of an existing cataract
- High or low pressure in the eye
- Need for repeated eye surgeries
- Vision loss, although rare
Life after diabetic retinopathy surgery
After diabetic retinopathy surgery, patients need to rest for 2 to 4 weeks. It will be weeks before patients can safely start driving.
Patients will need help from their health care provider to learn how to hold their head while awake and how to sleep correctly. Various pillows can be tried to help keep the head in the correct position.
It is possible for the eye to be swollen or slightly irritated after surgery. For this reason, redness or bruising may be seen for a while. It is important to use the prescribed eye drops appropriately. In addition, vision may be impaired for a few days after the operation.
What should people with diabetic retinopathy pay attention to?
The following are some of the things diabetic retinopathy patients can do to prevent the condition from worsening.
- Keeping blood pressure, blood sugar and lipids under control
- No smoking and alcohol use
- In case of sudden changes in vision, consult a doctor
- Even if there are no symptoms, diabetics should have regular eye checks
Risk factors for diabetic retinopathy
Everyone with diabetes can develop diabetic retinopathy. The risk of developing the disease can be increased by the following factors.
- Having diabetes for a long time
- Poor control of blood sugar levels
- High cholesterol
- Hypertension
- Pregnancy
- Tobacco use
- Be Black, Hispanic or Native American
Stages of diabetic retinopathy
Diabetic retinopathy is divided into two stages according to the severity of the disease.
Nonproliferative diabetic retinopathy (NPDR)
In the early stages of diabetic retinopathy, the walls of the blood vessels in the retina weaken. These small bulges in the blood vessels are known as micro aneurysms. Fluid or blood can leak into the retina through these bulges. This leakage not only causes the macula, the central part of the retina, to swell, but also causes the larger retinal vessels to dilate.
This change makes the size of the blood vessels irregular. When more blood vessels become blocked, symptoms begin to appear. In some cases, retinal blood vessel damage causes fluid or edema to accumulate in the macula. The development of edema usually causes visual impairment. In cases of severe blockage or muscle involvement, complete loss of vision is possible.
Proliferative diabetic retinopathy (PDR)
Proliferative diabetic retinopathy, an advanced form of diabetic retinopathy, occurs when damaged blood vessels become completely blocked and abnormal blood vessels grow in the retina. These newly formed blood vessels are extremely fragile and can leak into the vitreous, the jelly-like substance that fills the center of the eye, causing the retina to detach from the back of the eye.
Retinal detachment is characterized by blurred vision or dark areas in the vision. Untreated detachment can lead to blindness. In addition, pressure in the eyeball can increase if new blood vessels disrupt the normal flow of fluid out of the eye. This buildup can damage the optic nerves that carry images from the eye to the brain, leading to neovascular glaucoma.