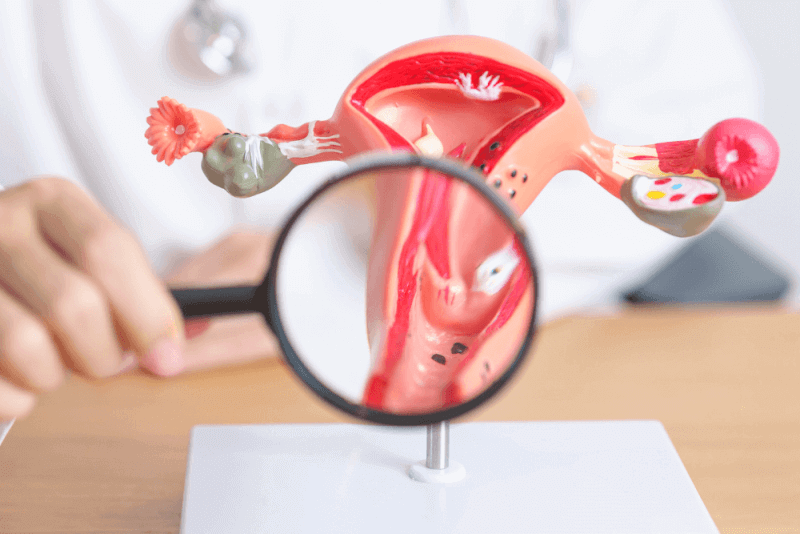
What is Endometrial Hyperplasia?
Also known as endometrial hyperplasia, endometrial thickening is the thickening of the lining of the uterus, leading to heavy or abnormal bleeding. Atypical endometrial hyperplasia is one of the factors that increases the risk of endometrial cancer and uterine cancer.
This condition tends to occur during or after menopause. Progestin therapy can help reduce symptoms. If there is a risk of cancer, removing the uterus may be considered.
Endometrial hyperplasia involves the thickening of the uterine lining, also known as the endometrium. This lining is shed during the menstrual cycle. It is also the tissue in which the fetus grows during pregnancy. In some women, endometrial hyperplasia can lead to endometrial cancer, most of which are uterine cancers.
Types of Endometrial Hyperplasia
Endometrial hyperplasia is classified according to the type of cell changes in the endometrial lining. Some types of endometrial hyperplasia greatly increase the risk of cancer, while others do not pose a cancer risk.
Simple or Complex Endometrial Hyperplasia (without atypia)
This type of endometrial thickening has normal-looking cells that are unlikely to be cancerous. This condition may resolve without treatment, or doctors may recommend hormone therapy.
Simple or Complex Atypical Endometrial Hyperplasia
If the type of endometrial hyperplasia is atypical, the likelihood of it turning into cancer is high. Without treatment, the risk of uterine cancer increases.
The terms simple or complex can be used in classification. Simple and complex refer to the patterns seen when looking at the cells.
Diagnosis Criteria for Endometrial Hyperplasia
Many different reasons can cause abnormal menstrual bleeding. Therefore, some tests are conducted to determine the causes of abnormal bleeding. These tests include:
- Ultrasound
- Biopsy
- Hysteroscopy
Symptoms of Endometrial Hyperplasia
The symptoms that can be seen in people with endometrial hyperplasia include:
- Abnormal menstrual bleeding
- Bleeding between periods
- Menstrual cycle lasting less than 21 days
- Heavy menstrual bleeding
- Bleeding after menopause
- No menstruation
Most of the above-mentioned symptoms are commonly seen in people going through menopause. Transition to menopause usually means irregular menstrual periods or skipped periods and irregular bleeding. Endometrial hyperplasia can cause pelvic and abdominal pain. In addition, pain during sexual intercourse may also occur.
Causes of Endometrial Hyperplasia
People with endometrial hyperplasia produce too much estrogen and not enough progesterone. These hormones play a role during menstruation and pregnancy. During ovulation, estrogen causes the endometrium to thicken; progesterone helps the uterus prepare for pregnancy.
If pregnancy does not occur, the progesterone level drops. The drop in progesterone triggers the shedding of the uterine lining during the menstrual period. People with endometrial hyperplasia produce very little progesterone, preventing the shedding of the endometrial lining. Instead, the lining continues to grow and thicken. The cells that make up the lining can become irregular and clump together.
Risk Factors for Endometrial Hyperplasia
The likelihood of endometrial hyperplasia increases in people who are perimenopausal or menopausal. Rarely, it can also be seen in people under the age of 35. Factors that increase the risk of endometrial hyperplasia include:
- Certain breast cancer treatments
- Diabetes
- Early onset of menstruation or late menopause
- Family history of ovarian, uterine, or colon cancer
- Gallbladder disease
- Estrogen hormone therapy
- Not getting pregnant
- Smoking
- Long history of irregular or absent menstruation
- Pelvic radiation
- Weakened immune system due to autoimmune disease or medications
Complications of Endometrial Hyperplasia
Some types of endometrial hyperplasia can cause abnormal and heavy bleeding that can make people anemic. Failure to treat atypical endometrial hyperplasia significantly increases the risk of cancer. Additionally, about 30% of people with untreated complex atypical endometrial hyperplasia develop cancer.
Treatment Methods for Endometrial Hyperplasia
A significant part of the treatment for endometrial hyperplasia involves administering the hormone progestin. Progestin is a synthetic version of the hormone progesterone, which is deficient in the body. Progestin is administered in various forms, including:
- Oral progesterone therapy
- Progesterone-releasing intrauterine device
- Injection
- Vaginal cream or gel
Endometrial Hyperplasia Surgery
In some cases, patients may need to have their uterus removed. This is especially recommended if the condition worsens or cancer cells develop. Surgery may also be recommended if the progestin treatment administered to some patients does not yield results.
Surgical Methods for Endometrial Hyperplasia
The surgical method used for endometrial hyperplasia is hysterectomy. This operation involves the surgical removal of the uterus and cervix.
Depending on the additional issues present in the patient, it may be possible to remove only the uterus, or to remove the uterus, fallopian tubes, and ovaries.
Hysterectomy surgeries can be performed vaginally or using the laparoscopic method. The steps involved in a vaginal hysterectomy include:
- The uterus is removed through an incision made at the top of the vagina.
- No external incisions are made.
- Absorbable stitches are placed inside the vagina.
- This method has fewer complications and the fastest recovery time.
In laparoscopic hysterectomy surgeries, several small incisions are made around the navel, and surgical instruments are inserted. The uterus is then removed in small pieces through these incisions into the vagina. Complete recovery takes less time than vaginal hysterectomy, and patients feel less discomfort.
Finally, due to technological advancements, abdominal hysterectomy is rarely preferred. In these operations, a 6 to 8-inch incision is made in the lower abdomen, and the uterus is removed. It is a type of surgery that is applied when the uterus is enlarged or when cancer is involved, as it causes a long recovery period.
Benefits of Endometrial Hyperplasia Surgery
For people with persistent pelvic pain or irregular bleeding, having a hysterectomy can help achieve a better quality of life. Especially in people with a high risk of uterine cancer, it significantly reduces this risk and can potentially save patients' lives.
Complications of Endometrial Hyperplasia Surgery
Side effects of endometrial hyperplasia surgery include vaginal discharge and irritation at the incision site. If the ovaries are also removed during a hysterectomy, menopausal-like symptoms are observed. These include:
- Hot flashes
- Vaginal dryness
- Loss of libido
- Insomnia
Additionally, it is not possible for women to menstruate or get pregnant after hysterectomy surgery.
Complications caused by the surgery include:
- Blood clots
- Severe infection
- Bleeding
- Bowel obstruction
- Opening of internal stitches
- Urinary tract injury
- Complications related to anesthesia
Recovery Process of Endometrial Hyperplasia
The length of hospital stay after hysterectomy surgery depends on the surgical method. Patients should start walking as soon as possible to ensure they are monitored and to confirm that there are no signs of complications such as blood clots or bleeding.
After abdominal hysterectomy surgery, patients may need to stay in the hospital for a few days. One night of hospital stay is usually sufficient after vaginal and laparoscopic hysterectomy.
Recovery time after vaginal and laparoscopic surgeries is 2 to 4 weeks. Recovery after abdominal hysterectomy can take up to 6 weeks. Patients should receive instructions from their doctors on how to care for themselves after surgery.
General post-hysterectomy instructions include:
- It is normal to experience light vaginal bleeding for 1 to 6 weeks after surgery. Hygienic pads are necessary for this.
- Heavy lifting should be avoided for 6 weeks after surgery.
- Tampons and similar vaginally inserted equipment should not be used for 4 to 6 weeks after surgery.
- Sexual intercourse should be avoided for 6 weeks after surgery.
- Showers can be taken after surgery. The incision site can be washed with soap and water. No bandaging is necessary over the incision. If surgical strips were used, they should fall off within a week. If staples were used to close the stitches, they need to be removed by a healthcare professional.
- Driving can be resumed 2 weeks after surgery, once the pain medication is no longer needed.
- Depending on how they feel, patients can return to their exercise routines within 4 to 6 weeks.
- Patients can usually return to work within 3 to 6 weeks, depending on the type of work they do.