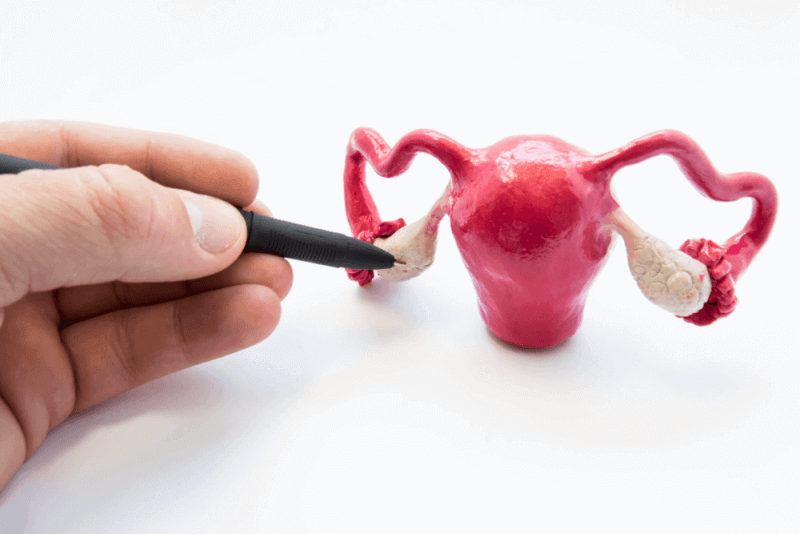
What is endometrial polyp?
Growths that adhere to the inner wall of the uterus and expand into the uterus are called uterine polyps. Uterine polyps, also called endometrial polyps, are the result of overgrowth of cells in the inner layer of the uterus. These polyps are usually benign, but in some cases they can be cancer cells. Some polyps can be characterized as precancerous polyps.
Endometrial polyps range in size from a few millimeters to several centimeters. They are attached to the uterine wall by a wide base or a thin stalk. The patient may have more than one uterine polyp. In some cases, endometrial polyps, which usually remain in the uterus, can slip through the cervix into the vagina. Although they are usually seen in women who have reached or completed menopause, they can also occur in younger women.
Endometrial polyp diagnosis
The following tests are used to diagnose endometrial polyps.
Trans vaginal ultrasound
A stick-like device inserted into the vagina emits sound waves to create an image of the uterus. In this image, polyps are clearly visible as well as thickened endometrial tissue.
A procedure called hysterosonography can be used to see the inside of the uterus more clearly. In this procedure, saline is injected into the uterus through a small tube inserted through the cervix. This salty water, called saline, allows the uterus to expand and be seen more clearly
Hysteroscopy
A lighted telescope called hysteroscopy is placed through the cervix into the uterus to visualize the inside of the uterus.
Endometrial biopsy
A suction catheter is inserted through the cervix into the uterus to collect the necessary tissue samples. These samples are then analyzed in laboratory environments. These samples are especially applied to detect cancer cells.
Causes of endometrial polyps
Hormonal factors are known to play a role in the formation of endometrial polyps. Uterine polyps are particularly sensitive to estrogen. Therefore, they grow in response to estrogen produced in the body.
Symptoms of endometrial polyps
Symptoms caused by endometrial polyps include
- Infertility
- Vaginal bleeding after menopause
- Heavy menstrual periods
- Bleeding between menstrual periods
- Unpredictable periods of varying length and severity
- Unusually heavy discharge between menstrual periods
- Bleeding after intercourse
Some patients have no symptoms, while others may experience mild bleeding or spotting.
Endometrial polyp treatment methods
Endometrial polyp treatments can be performed in 3 different ways. The first of these treatments is the waiting period. Close follow-up of patients with small polyps, especially those with asymptomatic polyps, may be recommended to monitor the development of the disease. Because these polyps can heal on their own.
Medication
Certain hormone therapies can be administered in medication form to reduce symptoms caused by polyps. However, these medications provide short-term solutions. Thus, when the medication is discontinued, the symptoms persist.
Endometrial polyp surgery
Hysteroscopy, which allows visualization of the inside of the uterus during hysteroscopy, makes it possible to remove polyps. The removed polyps are then sent to the laboratory for further examination.
Patients are lightly or completely sedated during the removal of endometrial polyps. The gynecologist is then guided through the vagina, cervix and uterus by hysteroscopy. Gas or saline is given to inflate the uterus and provide better vision. Gynecologists then remove the polyps with special scissors, a laser or other device that uses electricity.
Since the procedure is performed through the vagina, patients do not need to make any incisions. Patients are usually discharged after the procedure. However, in some cases patients need to move to the hospital overnight
On average, it takes 2 weeks for patients to fully recover after surgery. During this time, patients should not lift or push heavy objects. In addition, patients who are physically demanding should consult their doctors.
Benefits of endometrial polyp surgery
Uterine polyp surgery has several advantages for patients. This primarily includes improving fertility and pregnancy outcomes. Since uterine polyps prevent pregnancy, increase the risk of miscarriage and cause premature birth, surgical removal helps patients to have a healthy pregnancy period.
Endometrial polyp surgeries also help to reduce symptoms and improve the quality of life of patients. Because heavy bleeding in uterine polyps can cause anemia and fatigue in patients. It is possible to normalize bleeding by removing the polyps. This reduces the risk to patients' mothers
Finally, removal of polyps minimizes the risk of future complications and health problems. Because uterine polyps can develop into cancer and cause inflammation in the uterus.
Complications of endometrial polyp surgery
Complications that may occur after hysteroscopy include the following.
- Infection
- Bleeding
- Pelvic inflammatory disease
- Uterine rupture
- Damage to the cervix
- Complications from the fluid or gas used to dilate the uterus
These complications are rare but need to be taken into account. In addition, mild vaginal bleeding and cramps may occur for 1 to 2 days after the procedure. Other complications that may occur in the patient include the following.
- Bloating in the bladder
- Inflammation of the cervix
- Vaginal discharge
Life after endometrial polyp surgery
Among the changes that can be seen in patients during the recovery process after endometrial polyp surgery are the following.
- After the operation, some women experience discharge and spotting that persists for several weeks. The severity of the discharge and spotting decreases over time.
- Although patients feel well after surgery, they are advised to lift heavy objects for a few weeks.
- Unless otherwise advised by experts, sexual intercourse and bathing should be avoided.
- It takes 2 weeks for full recovery to be achieved.
Risk factors for endometrial polyps
Risk factors affecting the development of endometrial uterine polyps include the following.
- Hormone therapy for menopausal symptoms
- Being perimenopausal or postmenopausal
- Taking full oxygen, which is one of the provinces of drug treatment for breast cancer
- Being obese
- Age is the most important determinant for the occurrence of uterine polyps. The risk of uterine polyps increases as menopause approaches. For this reason, it is more common in people between the ages of 40 and 50 and is rarely seen in people under the age of 20.
- Having high blood pressure
- Lynch syndrome
- Cowden syndrome
Types of endometrial polyps
The following criteria are used to classify endometrial polyps.
- Number of polyps
- Size of polyps
- Their position in the uterus
- Implantation base features
- Histological features












G** O** | 02 Apr 2025