A stroke occurs when the brain's blood vessels are blocked or ruptured, leading to a lack of oxygen and resulting in damage to the brain. The severity of the damage varies depending on the affected area of the brain. In some patients, minor facial expressions may be affected, while in others, the consequences can be as severe as death.
What is Hemiplegia?
Hemiplegia is the term used to describe the neurological or physical damage that remains after a stroke. Although often confused with a stroke, hemiplegia is actually a result of it. The most common consequence of a stroke is the loss of muscle strength due to neurological damage, and hemiplegia is the most frequently encountered symptom in these clinical scenarios.
Right Hemiplegia
This term is used to describe paralysis on the right side of the body, typically caused by issues in the right nervous system. The most common cause of right hemiplegia is partial spinal cord injuries. Due to the severed nerves, the right side of the body completely loses function, while the left side remains unaffected.
Left Hemiplegia
Left hemiplegia refers to paralysis caused by an issue affecting the left side of the body. The most common cause is spinal cord injuries. Depending on the nerves affected by the injury, the left side loses function, while the right side may not experience any loss of function.
Types of Hemiplegia
Hemiplegia is classified into different types based on the affected areas and symptoms. The types of hemiplegia include the following:
Alternating Hemiplegia
Also known as crossed hemiplegia, this type involves ipsilateral cranial nerve paralysis and contralateral hemiplegia or hemiparesis of the extremities. The most characteristic feature of this type is recurrent paralysis attacks on one side of the body. It can occur in various forms and may also result from a unilateral brainstem lesion that affects both upper and lower motor neurons.
Upper Alternating Hemiplegia
Also known as Weber syndrome, upper alternating hemiplegia presents with several distinctive symptoms, including:
- Contralateral hemiparesis of the limb and facial muscles, along with weakness in one or more muscles controlling eye movement on the same side.
- Loss of eye movement due to damage to the oculomotor nerve fibers.
- Increased weakness in both upper and lower extremities.
Middle Alternating Hemiplegia
Also known as Foville syndrome, this type is characterized by weakness in the extremities on the opposite side of the affected area, accompanied by paralysis of the extraocular muscle, particularly the lateral rectus, indicating a lesion in the caudal and medial pons involving the abducens nerve root and corticospinal fibers.
Lower Alternating Hemiplegia
This type typically involves paralysis of the ipsilateral side of the tongue muscles. When the tongue is extended, it deviates towards the affected side. These symptoms indicate a lesion in the medulla involving the corticospinal fibers and the hypoglossal nerve roots.
Cerebral Hemiplegia
Also known as spastic hemiplegia, this type typically results from damage to the area of the brain responsible for movement. It is one of the spastic cerebral types.
This condition affects children before birth, during birth, or in the first few years of life. Children with cerebral hemiplegia may have difficulty with movements such as walking and reaching for objects. Some children may also experience problems such as epilepsy and attention deficit.
Spinal Hemiplegia
Also known as Brown-Séquard syndrome, spinal hemiplegia occurs due to damage to one side of the spinal cord. Paralysis occurs on the side of the injury, while there may be a loss of pain and temperature sensation on the opposite side of the body.
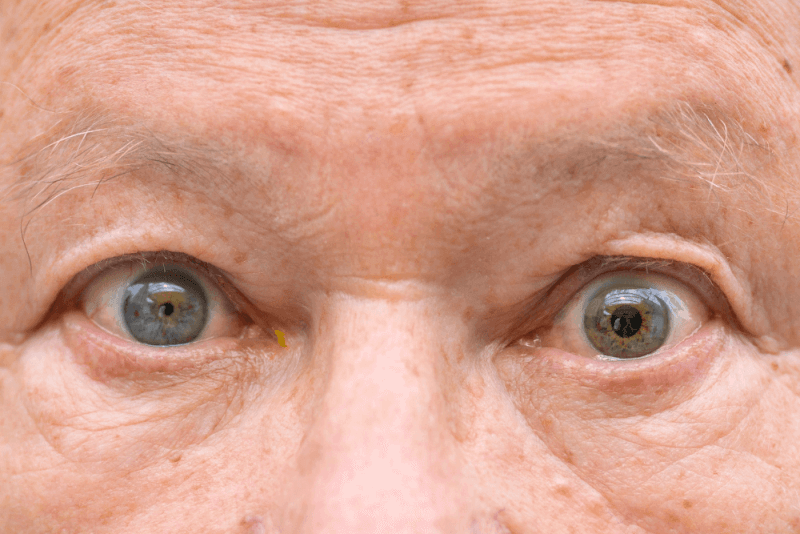
Facial Hemiplegia
Individuals with facial hemiplegia experience paralysis of the muscles on one side of the face. Facial hemiplegia may also be accompanied by mild hemiplegia in other parts of the body.
Symptoms of Hemiplegia
The symptoms of hemiplegia vary depending on the affected areas of the brain. The most common symptoms include the following:
Spasticity
Spasticity, a condition of excessive muscle contraction, is often seen in the early stages of the disease. If the arms are affected, it can cause flexion at the elbow. When spasticity occurs in the legs, it can lead to extension, causing the knee joint to move in the opposite direction. If spasticity persists for a long time, it can result in muscle stiffness, a condition known as rigidity.
Dyskinesia
Dyskinesia, involuntary muscle movements, occurs due to prolonged muscle contractions.
Tremor
Tremor, an involuntary shaking or trembling, is another symptom associated with prolonged muscle contractions.
Ataxia
Ataxia, which occurs in almost every stage of hemiplegia, is characterized by a lack of coordination in speech and walking. This coordination disorder can be seen in all complex movements.
Paralysis
In some patients, hemiplegia can lead to complete loss of muscle strength, a condition known as paralysis.
Apraxia
Apraxia, another symptom seen in hemiplegia patients, is the inability to perform movements despite having the physical ability to do so.
Mental and Psychological Disorders
Some patients may experience mental disorders, along with psychological and psychosocial dysfunctions.
Causes of Hemiplegia
Since hemiplegia results from a stroke, the factors that cause a stroke also contribute to the development of hemiplegia. Hemiplegia can develop due to a variety of causes.
Age
Approximately 75% of stroke patients are over the age of 65, making age a significant risk factor. The risk of stroke doubles every 10 years after age 55, highlighting the importance of regular neurological check-ups for individuals over 50.
Heart Diseases
Heart diseases increase the risk of stroke by causing problems such as narrowing and hardening of the brain's blood vessels. Conditions like atrial fibrillation, if untreated, can increase the risk of stroke fivefold. However, using oral anticoagulants can reduce the risk by 70%. Regular monitoring is essential for individuals with heart rhythm disorders.
Diabetes
People with diabetes are more likely to experience artery blockages, hypertension, hyperlipidemia, and obesity. Consequently, the risk of stroke is twice as high in women and 1.8 times higher in men.
Hypertension
Hypertension is a major risk factor for systemic strokes, which occur when blood circulation in the brain's arteries is partially or completely blocked. Hypertension accounts for about 60% of stroke cases, but controlling hypertension can reduce this risk by 40%.
Smoking
Smoking is extremely harmful to the cardiovascular system and doubles the risk of stroke. Quitting smoking can reduce this risk to levels similar to those in the general population within 2 to 4 years.
Diets High in Animal Products
Diets rich in animal products can damage blood vessels and contribute to obesity.
Insufficient Physical Activity
Decreased physical activity, particularly with age, is a factor that increases the risk of stroke.
How is Hemiplegia Diagnosed?
Hemiplegia is typically diagnosed through clinical examination. Symptoms such as spasticity, sensory-motor dysfunction, and muscle contractions following a stroke history are usually sufficient for diagnosis. Additional symptoms like tremors, body pain, and difficulty performing complex movements can also help confirm the diagnosis.
Treatment of Hemiplegia
Treatment of hemiplegia begins immediately after a stroke. Once the patient's condition stabilizes, each muscle group is assessed to determine whether hemiplegia has developed. The affected muscle groups are identified, and a treatment plan is formulated.
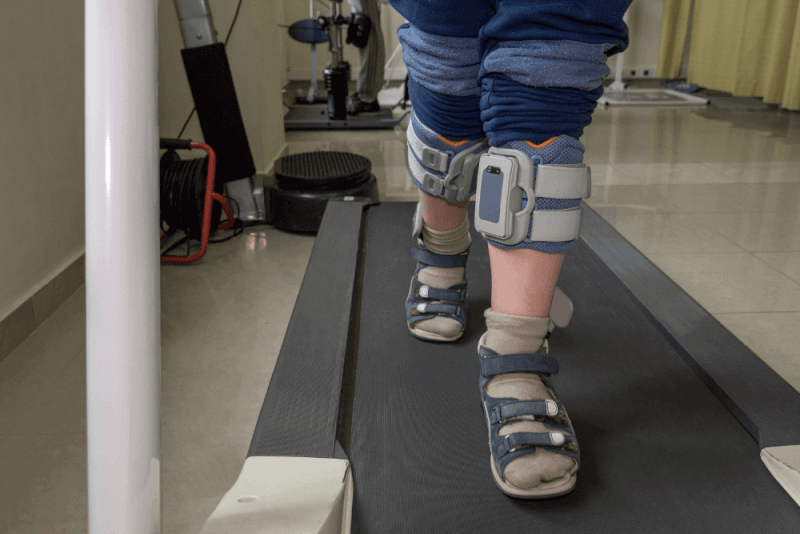
The first step in treating hemiplegia is physical therapy. With the help of specialized physiotherapists, planned exercises aim to maximize muscle strength and coordination, preserve muscle function, and maintain and sustain normal joint movements. Physical therapy plans are tailored to each patient.
Physical Therapy
Physical therapy is the initial treatment for all types of hemiplegia. Before starting physical therapy, patients should be evaluated not only physically and neurologically but also mentally and psychologically, as the goal is to optimize muscle function.
Acute Rehabilitation
The acute rehabilitation phase, the first stage of physical therapy, involves passive range of motion exercises for the patient's joints. The goal of this phase is to improve the patient's ability to sit up in bed. The exercises include:
- Passive
- Assisted active
- Active
- Active-resisted
- Progressive resistance methods
Chronic Rehabilitation
The next phase, chronic rehabilitation, aims to help patients regain daily living skills. During this phase, acute rehabilitation methods continue, along with additional techniques. Techniques used during chronic rehabilitation include:
- Rolling
- Assisted sitting up
- Knee locking
- Weight-bearing
- Weight shifting
- Balance
- Gait training
Additional techniques may be applied based on the patient's needs.
Hemiplegia Exercises
Since hemiplegia causes muscle weakness, patients have less control over their arms and legs. It is important to continue with regular physical therapy and exercises to strengthen muscles and improve balance. However, consulting a doctor before starting any exercise is crucial.
Standing Exercises
A significant number of hemiplegia patients experience at least one fall within the first 6 months of recovery. Therefore, exercises aimed at improving balance and strengthening leg muscles are essential. The steps include:
- Begin by kneeling next to a chair.
- Then, place weight on the foot closest to the chair.
- Slowly sit down on the chair.
- Repeat the same steps for the other foot.
Shoulder, Arm, and Hand Exercises
Various exercises are available to address weakness in the shoulders, arms, and hands, helping these muscles regain their function.
Hands
Hand exercises are crucial for fine motor skills and are used in many daily activities. A simple exercise involves crumpling a piece of A4 paper, which helps strengthen and restore function to the small muscle groups in the fingers. Both hands should be used equally during the exercise.
Shoulder Flexibility
This exercise, which helps strengthen shoulder and elbow muscles and straighten the elbow, should be repeated 10-12 times a day. The steps to increase shoulder joint flexibility are:
- Lie on your back.
- Hold the ends of a resistance band firmly.
- Lower one arm straight to the side. Use the other hand to lift the resistance band overhead, keeping the elbow straight.
Shoulder Exercise
This exercise is designed to maintain shoulder range of motion and ease turning in bed. It should be performed 15-20 times daily. If severe pain is felt, the range of motion should be limited. Another shoulder flexibility exercise involves the following steps:
- Lie on your back.
- Clasp your hands together at waist level.
- Reach your hands first to the left, then to the right.
Sitting Trunk Rotation
This exercise, which increases shoulder flexibility and function, also reduces trunk stiffness and supports the rotation necessary for walking. It helps improve balance and walking control. The exercise should be repeated 8-10 times twice a week. The steps are:
- Sit upright on a chair.
- Clasp your hands together and reach for your left toe.
- Then, with hands still clasped, reach overhead on the right side. Repeat the movement for the other side.
Sitting Weight-Bearing Elbow Flexion and Extension
This exercise helps strengthen shoulder muscles and also aids in straightening the elbow. It should be repeated 15-20 times. However, it should only be performed if the paralysis has fully healed. The steps are:
- Sit on the floor with legs extended.
- Gently twist your waist and place your palm on the floor.
- Then, control your movement and place your elbow on the floor without lifting your palm.
Supine Elbow Flexion
This exercise helps straighten the elbow and strengthen muscles. It should be repeated 20-25 times a day. The steps are:
- Lie on your back with legs naturally spread.
- Place a small rolled-up towel under the elbow.
- With the arm straight, bend the elbow to lift the hand upward and then lower it.
Supine Shoulder Flexion Active Range of Motion
This exercise strengthens the muscles that stabilize the shoulder. It should be repeated until the muscles are tired. The steps are:
- Lie on your back.
- Extend your arms naturally at your sides.
- Then, without bending the elbow, lift the arm upward.
- In this position, make a fist with your hand. Lift the shoulder off the ground while the arm is raised.
- Lower the arm straight down to the ground.
Supported Reach and Grasp
This exercise is suitable for those who have difficulty reaching objects and is designed to strengthen the shoulder, elbow, and wrist muscles. It should be repeated 20 times or until the arm muscles are tired. The steps are:
- Position the arm on the table with the elbow resting on it.
- Slide the hand forward on the table. Meanwhile, open the hand and extend the fingers forward.
Leg, Ankle, and Foot Exercises
In hemiplegia patients, the affected areas often include the lower parts of the body. Strengthening these areas helps improve the patient's mobility. The following are some exercises for the leg, ankle, and foot:
Bridge Weight Lifting
This exercise, which helps maintain balance for proper walking technique, also improves coordination. The exercise should be repeated until the leg muscles are tired. The steps are:
- Lie on your back.
- Bend the legs at the knees and place the feet flat on the ground.
- Ensure that the lower back is fully in contact with the ground.
- Place the arms flat on the ground with palms facing down for balance.
- Lift the hips upward.
- While the hips are raised, push them to the right and left.
- Return the hips to the center position and lower them back down.
Calf Stretching
This exercise is designed to maintain ankle mobility, which is essential for walking. If pain is felt during the exercise, do not force it. Hold the position for as long as the patient can tolerate, and perform the exercise twice a week. The steps are:
- Place your hands on the back of a chair for support.
- Step one foot back.
- Bend the front knee and stretch the back calf muscle.
- Then, repeat the movement for the other leg.
Mini Lunge
This exercise strengthens the muscles in the hips, legs, and core, making it easier to shift weight correctly. It should be repeated 8-10 times on each side. The steps are:
- While standing, take a big step forward.
- Ensure that the feet are pointing straight ahead.
- Place your hands on your hips for balance.
- Bend the knees to engage the muscles. Work the right and left legs alternately.
Side-Lying Knee Flexion
This exercise helps improve knee control, which is necessary for walking. It should be repeated 15-20 times or until the hip muscles become difficult to control. The steps are:
- Lie on your side.
- Bend the arm at the elbow and place it under your head.
- Bend the top leg at the knee.
- Then switch to the other leg.
Side-Lying Hip Flexion
This exercise simulates the movement needed for walking, helping to improve hip and knee movements. It also makes it easier to move to the edge of the bed before sitting up. The exercise should be repeated 15-20 times or until the hip muscles become fatigued. The steps are:
- Lie on your side with the affected side on top.
- Support your head with your arm.
- Bend the affected leg at the knee and bring it forward to a 90-degree angle.
Supported Single-Leg Mini Squat
This exercise improves weight shifting and knee control necessary for walking, while also strengthening the leg muscles. It should be performed 8-10 times or until the leg becomes tired. The steps are:
- Stand upright next to a table.
- Support yourself with one hand on the table.
- Step the leg closest to the table back and stand on your toes.
- Lower yourself down without losing position.
Supported Small Steps
This exercise strengthens the muscles in the hips, thighs, and legs. It should be performed twice a week, with 10-15 repetitions. The exercise requires a step that provides support on both sides. The steps are:
- Hold onto the support bars of the step.
- Step onto the step with one foot.
- Keep the other foot back and off the ground.
- Stand upright on the step and lower the elevated foot to the ground.
Supported Standing Hip Abduction
This exercise strengthens the hip and leg muscles, improving weight control during walking. It should be repeated 10-12 times for each leg. The steps are:
- Stand upright facing a table.
- Support yourself with the table and lift one leg to the side.
- Ensure that the knee remains straight during the lift.
Supine Heel Slides
This exercise, which prepares for walking, helps improve hip and knee control. It should be repeated 20-25 times or until the hip muscles are fatigued. The steps are:
- Lie on your back.
- Extend your legs.
- Slide the affected leg toward your hip, bending it at the knee until the foot is flat on the ground.
Supine Knee-to-Knee Trunk Rotation
This exercise supports pelvic, hip, and knee movement, while also reducing stiffness in the spine, making it easier to turn in bed. It should be repeated 15-20 times. The steps are:
- Lie on your back.
- Position your legs with feet flat on the ground.
- With the knees together, twist from the waist and try to touch the knees to the ground. Return to the center position.
Supine Leg Crossover
This exercise helps improve hip control in preparation for walking. If the leg muscles become fatigued, the exercise should be stopped. The steps are:
- Lie on your back.
- Spread your feet slightly wider than shoulder-width apart. Move one leg so that it crosses over the outside of the other knee.
- Return the crossed leg to its original position.
Supported Mini Squat
This exercise strengthens the leg muscles needed for walking, endurance, and standing up from a seated position. It should be repeated 15-20 times. The steps are:
- Stand facing the back of a chair.
- Squat down by bending your knees while holding onto the back of the chair for support.
- Stand back up straight.
Balance Exercises
To walk, patients need to maintain good balance. Maintaining balance is important not only for walking but also for activities such as sitting and standing, as it helps prevent accidents and makes movements easier. Balance exercises include:
Dynamic Weight Lifting
This exercise, which helps improve balance and core muscle control, should be performed 20-30 times daily. The steps are:
- Sit upright in a chair with your feet flat on the ground.
- Lean your body first to the left, then to the right.
- Ensure that the muscles on the leaning side are stretching while the muscles on the opposite side are contracting.
Four-Legged Leg Slides
This exercise, which is part of the preparation for walking, helps improve balance, weight shifting, and control. It should be repeated 10-15 times on each side. The steps are:
- Position yourself on all fours with hands and knees on the ground.
- Open your hands and knees shoulder-width apart.
- Move forward to the left.
- Then, move backward to the right.
- Return to the starting position between each movement.
- Repeat the same movements for the other directions.
Single-Leg Stand
This challenging balance exercise requires holding the position for 30-60 seconds. It should be performed on both sides. To increase the difficulty, the eyes can be closed. The steps are:
- Stand upright with arms at your sides in a natural position.
- Lift one leg by bending the knee and hold it at a 90-degree angle.
- Then, lift the other knee.
Sit-to-Stand
This exercise, which strengthens the leg muscles, also enables the transition from a sitting position to standing. It is important to ensure that weight is distributed equally between both legs during the exercise. It should be repeated 15-20 times daily. The steps are:
- Sit at the edge of the chair with knees bent at a 90-degree angle and feet flat on the ground.
- Clasp your hands together and stand up.
- Stand fully upright and then sit back down in the chair.
Staggered Stance
This balance exercise requires holding the position for 30-60 seconds. It should be performed on both sides, and to increase difficulty, the eyes can be closed. The steps are:
- While standing upright, place one foot immediately in front of the toes of the other foot.
- Hold the position. Then return the foot to its original position and repeat the movement for the other foot.
Hemiplegia Recovery Process
Hemiplegia, which can be caused by life-threatening conditions, can also occur due to temporary causes such as migraines. Therefore, the recovery process varies depending on the cause. However, regardless of the cause, diagnosis is essential. If necessary, emergency medical intervention should be provided. The treatment will also vary depending on the cause.
During the recovery process, it is important to maintain a balanced and healthy diet. Maintaining an ideal weight is crucial. Additionally, patients with comorbid conditions such as type 2 diabetes or high blood pressure should manage these conditions well, as complications may arise otherwise.
Another important aspect of the recovery process is protecting against infections, particularly those affecting the eyes and ears.
Nutrition for Hemiplegia Patients
Since hemiplegia affects the central nervous system, and the nervous system uses glucose as fuel, it is important to maintain normal blood sugar levels in hemiplegia patients to preserve cognitive health.
To support the treatment of hemiplegia patients, their diet should be rich in B vitamins. Patients should include green leafy vegetables, legumes, fish, red meat, dried fruits, eggs, and whole wheat flour in their diet.
To maintain the effectiveness of medications used in treatment, hemiplegia patients should also include foods rich in vitamin K in their diet. These foods include dark leafy vegetables, soy oil, egg yolk, lentils, and liver.