What is a Hormonal IUD?
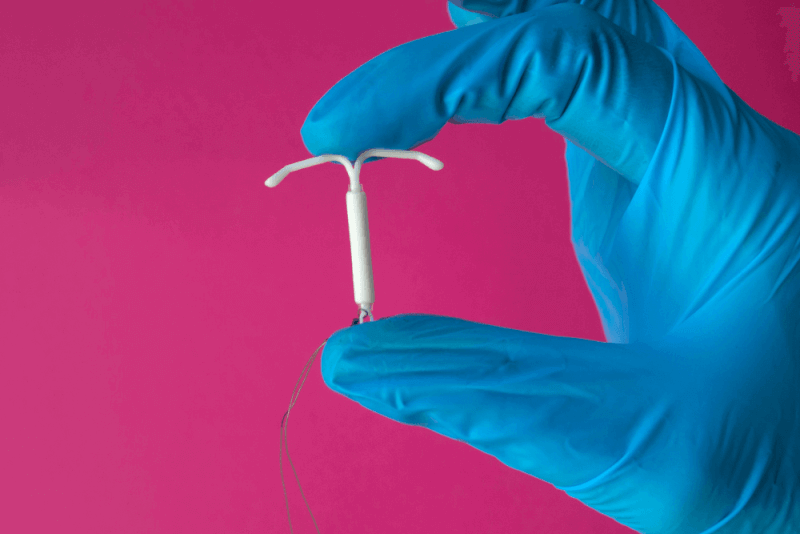
Also known as a hormonal intrauterine device, a hormonal IUD is a type of birth control placed in the uterus that uses hormones for long-term birth control. This T-shaped plastic device releases a type of progestin hormone. It prevents pregnancy through the following mechanisms:
- Thickening the mucus in the cervix to prevent sperm from reaching and fertilizing an egg.
- Thinning the lining of the uterus and partially stopping ovulation.
When is a Hormonal IUD used?
Reasons for using a hormonal IUD include:
- As a method of birth control
- Heavy menstrual bleeding
- Non-cancerous growths in the uterus
- Menstrual cramps and pain
- Anemia (low levels of healthy red blood cells)
- Endometriosis
- Abnormal growth of uterine tissue into the uterine wall muscles
- Abnormal growth of the endometrial lining
Who should not use a Hormonal IUD?
A hormonal IUD is not suitable for everyone. Individuals with the following conditions should avoid this method:
- Breast cancer or a history of breast cancer
- Abnormal uterus
- Cervical or uterine cancer
- Unexplained vaginal bleeding
- Liver disease
- Pelvic infection or current pelvic inflammatory disease
- Uterine conditions like fibroids that could interfere with IUD placement or retention
In addition, consultation with a doctor is required if you have the following conditions:
- Recent childbirth and breastfeeding
- Using any medications, including herbal products and supplements
- Blood clotting disorders
- History of stroke
- Diabetes
- High blood pressure
- Migraine
- Heart disease
- History of heart attack
How is a Hormonal IUD inserted?
During the procedure, a speculum is used to keep the vagina open. An antiseptic solution is applied to clean any bacteria in the vagina and cervix.
Special tools are used to stabilize the cervix and align it with the uterus. Doctors measure the depth of the uterus based on its size and shape.
The arms of the hormonal IUD are folded, and the device is placed inside an application tube. The tube is inserted into the cervical canal to place the IUD into the uterus. The tube is then removed, leaving the IUD in place.
The strings of the IUD are cut to ensure they do not protrude too much into the vagina. It should be possible to feel the trimmed strings.
Dizziness or fainting may occur during the procedure, along with a slower-than-normal heart rate. Cramping is also expected.
Signs of a Displaced Hormonal IUD
Factors that can cause a hormonal IUD to move include:
- History of pregnancy
- Insertion immediately after childbirth
- Heavy or prolonged menstrual periods
- Being under 20 years old
- Severe menstrual cramps
- Previous expulsion of an intrauterine device
Advantages of a Hormonal IUD
Advantages of using a hormonal IUD include:
- Always ready for use, no need to pause for birth control during intercourse.
- Can be used for emergency contraception if inserted within 5 days of unprotected intercourse.
- No need for partner involvement in birth control.
- Safe for use during breastfeeding.
- Provides protection for up to 8 years.
- Can be removed at any time.
- Fertility returns immediately after removal.
- Bleeding decreases after more than 3 months of use.
- About 20% of users stop having periods after one year of use.
- Reduces the risk of pelvic infections.
- Reduces severe menstrual cramps.
- Reduces pain caused by endometriosis.
- Reduces the risk of endometrial cancer.
Disadvantages of a Hormonal IUD
The following are disadvantages associated with hormonal IUDs. If these occur, specialists may recommend removing the IUD:
- Pelvic infection requiring the removal of the IUD.
- Significant increase in blood pressure, heart attack, or stroke.
- Severe cases of myopia.
- Swelling and irritation of the uterine lining.
- Pelvic pain during intercourse.
- Cervical or endometrial cancer requiring IUD removal.
Side Effects of a Hormonal IUD
Pregnancy occurs in less than 1% of users with a hormonal IUD, often as ectopic pregnancies. However, the risk is lower compared to those not using birth control. Side effects include:
- Risk of uterine perforation, especially if inserted immediately after childbirth.
- Headache
- Breast pain
- Acne
- Cramps or pelvic pain
- Irregular bleeding, especially in the first 3 months
- Mood changes
When should a Hormonal IUD be inserted?
Times for inserting a hormonal IUD include:
- During the menstrual cycle
- Immediately after terminating a pregnancy
- Immediately after vaginal or cesarean delivery
Precautions before getting a Hormonal IUD
Patients are examined and given a pelvic exam before getting a hormonal IUD. A pregnancy test is done to ensure the patient is not pregnant before the procedure.
Taking nonsteroidal anti-inflammatory drugs like ibuprofen an hour or two before the procedure can help reduce cramps.
Precautions after getting a Hormonal IUD
A follow-up pelvic exam may be done about a month after the procedure to ensure the IUD has not moved. Patients should check the IUD strings monthly. Post-procedure precautions include:
- Suspected pregnancy
- Heavier-than-usual vaginal bleeding
- Pelvic pain during intercourse
- Fever
- Vaginal sores
- Foul-smelling discharge
- Migraine
- Yellowing of the skin and eyes
- Infection
- Not feeling the IUD strings or feeling them longer than usual
- Feeling part of the IUD
Hormonal IUD and Sexuality
Both partners may feel the IUD strings during intercourse after insertion. Over time, the strings soften, and this sensation usually disappears. Pain during intercourse is possible, and if it occurs, consultation with a doctor is necessary.