30-Second Summary
- Liver transplantation is a surgical procedure in which a liver that can no longer function is removed and replaced with a whole liver from a deceased donor or a portion of a liver from a living donor.
- Liver transplantation is usually reserved as a last treatment option for individuals who experience severe complications due to end-stage chronic liver disease.
- In living donor transplants, a portion of a healthy organ is removed and transplanted into the patient. Thanks to the liver’s ability to regenerate, the transplanted organ returns to its normal size in a short period of time.
- Liver transplantation is a treatment option for individuals with liver cancer and liver disease whose conditions cannot be controlled by other treatment methods. Liver failure may occur rapidly or over a long period of time.
What is Liver Transplantation?
Liver transplantation is a surgical procedure in which a liver that can no longer function is removed and replaced with a whole liver from a deceased donor or a portion of a liver from a living donor.
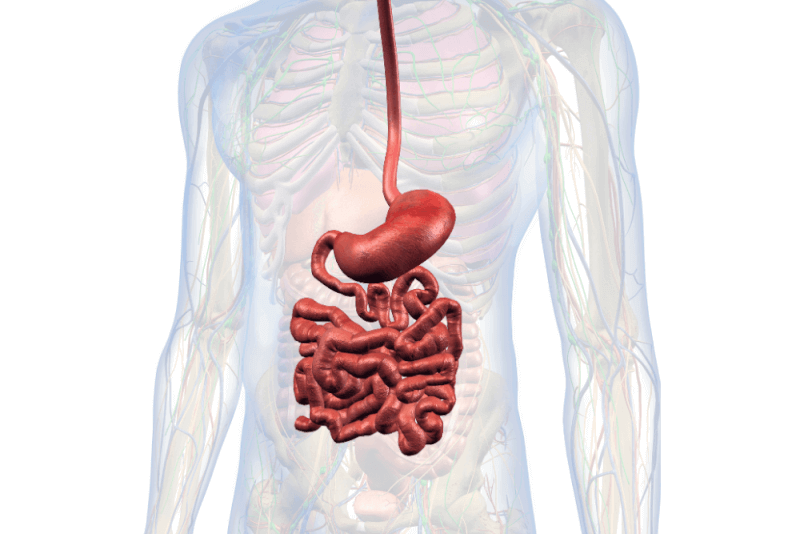
As the largest internal organ in the body, the liver performs many functions, including the following:
- Processing nutrients, medications, and hormones
- Producing bile to help the body absorb fats, cholesterol, and fat-soluble vitamins
- Producing proteins that help blood clot
- Removing bacteria and toxins from the blood
- Preventing infections
- Regulating immune responses
Liver transplantation is generally reserved as the last treatment option for individuals who experience serious complications due to end-stage chronic liver disease. It is also the most important treatment option in rare cases where liver damage occurs suddenly and severely.
Due to the number of people waiting for a liver transplant exceeding the number of cadaveric livers available, living donor liver transplantation is a common practice. In living donor transplants, a portion of a healthy organ is removed and transplanted into the patient. Thanks to the liver’s ability to regenerate, the transplanted organ returns to its normal size in a short time.
What is a Paired Liver Exchange Transplant?
Paired liver exchange surgery is also one of the liver transplant procedures. However, in these surgeries, donors give their livers to another patient due to incompatibility with their own recipients. The donor of the recipient who receives the liver also donates their liver to the other patient. This type of surgery can also be applied to other living donor transplant procedures, not just liver transplants. Since these operations are carried out simultaneously, they require extensive coordination. If one donor backs out, there is a risk of canceling all the surgeries.
Reasons for Liver Transplantation
Liver transplantation is a treatment option for individuals with liver cancer or liver disease whose conditions cannot be controlled by other treatment options. Liver failure can occur suddenly or over a prolonged period of time.
Rapid onset of liver failure within a few weeks is called acute liver failure. Acute liver failure is a rare condition that usually occurs as a complication of certain medications.Although liver transplantation is used in acute liver failure, it is more commonly the preferred treatment method for chronic liver failure.
Cirrhosis is the most common cause of chronic liver failure. When cirrhosis occurs, scar tissue replaces the typical liver tissue, and the liver cannot function properly. Factors causing cirrhosis, the leading cause of liver transplantation, include:
- Hepatitis B and C
- Alcoholic liver disease, which results from excessive alcohol consumption causing liver damage
- Non-alcoholic fatty liver disease, a condition that leads to inflammation or liver cell damage due to fat accumulation in the liver
- Genetic disorders affecting the liver, such as hemochromatosis (causing iron accumulation) and Wilson’s disease (causing copper accumulation in the liver)
- Diseases affecting the bile ducts, including primary biliary cirrhosis, primary sclerosing cholangitis, and biliary atresia. Biliary atresia is the most common cause of liver transplantation in children.
In addition, liver transplantation is a treatment option for certain types of cancer that develop in the liver.
Eligibility Criteria for Liver Transplantation
For a liver transplant to be performed, both the patient and the donor must meet appropriate eligibility criteria. Additionally, compliance with the national liver transplantation regulations is essential. Otherwise, patients cannot be placed on the transplant waiting list.
Although the legal requirements may vary by country, common conditions that must be met by patients include:
- Having acute or chronic liver failure
- Meeting the eligibility criteria for each type of cancer in cases where the transplant is due to cancer
- Absence of substance use disorders
- Absence of alcoholism
Patients deemed eligible for liver transplantation are referred to healthcare institutions capable of performing the procedure. Each healthcare institution has its own specific criteria. If the requirements of one institution are not met, another transplant center may be considered. When choosing a transplant center, patients should take into account the following:
- Obtaining information on the number and types of transplants performed annually by the center
- Learning about the survival rates of liver transplants at the center
- Understanding the costs incurred before, during, and after the transplant
- Inquiring about support services offered by the transplant center, such as support groups, accommodation, or travel planning assistance
- Getting informed about the technology used at the transplant center
If the transplant center finds the patient suitable, they also assess whether the patient meets their internal criteria. While each center has its own requirements, the goals of the evaluation process generally include the following:
- Ensuring the patient is healthy enough to undergo surgery
- Determining if the patient can tolerate lifelong medications post-transplant
- Checking for any other illnesses that may affect the success of the transplant
- Assessing whether the patient is willing and capable of adhering to medication instructions
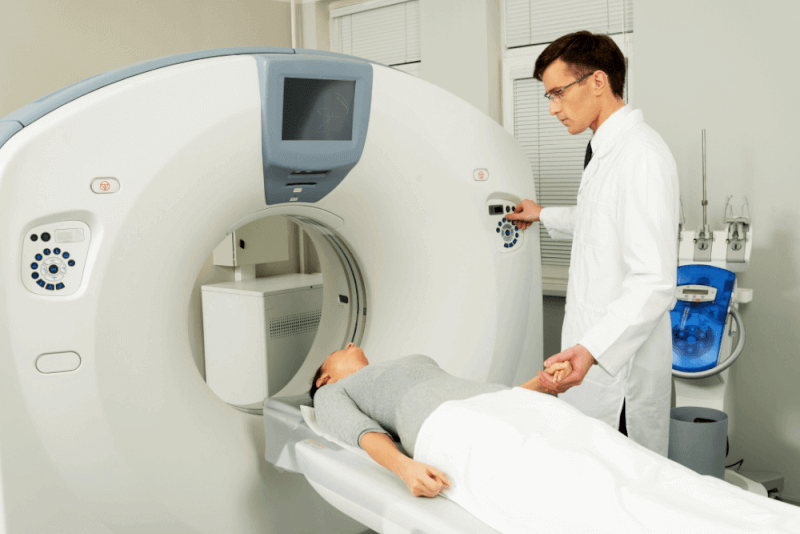
Tests that may be included in the patient evaluation process are:
- Blood and urine tests to assess the health of all organs, including the liver
- Imaging tests such as liver ultrasound
- Heart tests to evaluate cardiovascular health
- General health checkups including routine cancer screenings to detect other conditions that may affect transplant success
Additional evaluations may include the following:
- Assessment of the patient's diet and recommendations for healthy meal planning post-transplant
- Psychological evaluation to identify and treat underlying conditions such as depression and anxiety, and to ensure the patient fully understands the risks of liver transplantation
- Assessment of whether someone is available to care for the patient after the transplant
- Addiction counseling to help those struggling to quit alcohol, drugs, or tobacco
- Understanding the costs of post-transplant care and identifying what expenses are covered by insurance
In cases where the liver donor is a living donor, general conditions that must be met by the donor include:
- Whether the donation is being made voluntarily
- Whether the donor is of legal age
- The familial relationship between the donor and the recipient
- Compatibility of the donor’s blood type with the recipient’s
- Whether the donor has a healthy liver
How is Liver Transplantation Performed?
The procedures performed during liver transplantation vary depending on the donor. In cases where the transplant is performed from a deceased donor, the liver has a limited survival time outside the body, making it extremely important for patients to reach the transplant center as quickly as possible. After the patient is admitted, pre-operative evaluations are carried out rapidly, and the patient is quickly taken into surgery.
In cases of living donor liver transplantation, the surgery can be planned in advance. At this point, the general health status of the patient with liver failure is crucial. Both the patient and the donor must be in good health to undergo the surgery.
Liver Transplantation Process
Liver transplant surgeries are major operations. General anesthesia is administered to the patient during the surgery. During and immediately after the surgery, the surgeon will place tubes in various parts of the patient’s body to perform certain functions. The steps of the operation include:
- Establishing intravenous (IV) access to administer necessary fluids and medications
- Inserting a catheter into a vein in the neck or groin to allow healthcare providers to collect blood samples and continuously monitor blood pressure
- Inserting a tube into the windpipe through the mouth and connecting it to a mechanical ventilator. The ventilator helps the patient breathe during surgery and ensures automatic lung expansion
- Placing tubes in the abdomen to drain blood and fluids around the liver. A nasogastric tube inserted through the nose into the stomach allows gastric fluids to be drained
- Placing a catheter in the bladder to drain urine
The surgical stages are as follows:
- A long incision is made in the abdominal area to access the liver
- The liver is slowly detached from the ligaments attaching it to the abdominal wall. The bile duct and blood vessels connected to the liver are clamped
- The liver and gallbladder are removed
- The donor liver is placed
- The incision is closed
After Liver Transplantation
After a liver transplant, patients can expect the following:
- Patients are cared for in the intensive care unit for several days to closely monitor for any post-operative complications. Frequent tests are also conducted to ensure the liver is functioning properly.
- Once the patient is stable, they are transferred to a regular hospital room to continue recovery. Patients usually stay in this room for 5 to 10 days.
- After being discharged, patients must attend follow-up appointments frequently. In the first few weeks, check-ups are required several times a week. Later, testing is done less often.
Liver Transplantation and Complications
Liver transplant surgeries are procedures that involve significant complications. There are risks associated with the procedure itself as well as with the medications used to prevent rejection of the donor liver.
Risks related to the procedure include:
- Bile duct complications, such as leaks or narrowing of the bile ducts
- Bleeding
- Blood clot formation
- Failure of the transplanted liver
- Infection
- Rejection of the donated liver
- Mental confusion and seizures
Long-term complications may include the recurrence of liver disease in the transplanted liver.
Side effects of anti-rejection medications include:
- Bone thinning
- Diabetes
- Diarrhea
- Headache
- High blood pressure
- High cholesterol
Because anti-rejection medications suppress the immune system, individuals are at significantly increased risk of developing infections. Therefore, medications to fight infections may also be prescribed.
Risks for Liver Donors
Although live liver donation is considered a very safe operation, it still requires major surgery. Therefore, some complications may occur. These complications include:
- Allergic reaction to anesthesia
- Pain
- Discomfort
- Nausea
- Wound infection
- Bleeding that may require transfusion
- Blood clots
- Pneumonia
- Bile leakage
- Bile duct problems
- Hernia
- Scar tissue formation
- In rare cases, liver failure and the need for liver transplantation
- Death
Life After Liver Transplantation
It is perfectly normal for patients to experience stress before a liver transplant. Additionally, concerns such as fear of organ rejection after the transplant are also expected. During these times, receiving support from family members and close friends is extremely important. The transplant team may also recommend the following methods:
- Joining a support group for organ transplant recipients
- Sharing experiences on social media
- Utilizing rehabilitation services
- Setting realistic goals
- Educating oneself
Diet and Nutrition
After a liver transplant, adopting a balanced diet is essential to support recovery and help maintain a healthy liver. The transplant team will refer the patient to a dietitian to discuss nutritional and dietary needs.
Post-transplant diets should generally be low in salt, cholesterol, fat, and sugar. Additionally, alcohol should be avoided to prevent harm to the new liver.
Dietitians may also provide suggestions for various healthy food options and ideas. Their recommendations may include:
- Eating at least five servings of fruits and vegetables every day
- Avoiding grapefruit and grapefruit juice due to their interaction with immunosuppressive drugs
- Ensuring adequate fiber intake in daily meals
- Choosing whole grains over processed foods
- Consuming low-fat or fat-free dairy products to maintain optimal calcium and phosphorus levels
- Eating lean meats, poultry, and fish
- Following food safety guidelines
- Drinking enough water and other fluids daily
Exercise
After a liver transplant, incorporating exercise and physical activity into daily life is essential for improving both physical and mental health.
Patients should begin walking shortly after the transplant. As recovery progresses, daily physical activity should be gradually increased.
Low-impact exercises such as walking, cycling, or swimming, as well as activities that are enjoyable, are recommended. However, medical advice should be sought before starting any active routine.
Survival Rates After Liver Transplantation
The success rate of liver transplant surgeries is over 90%. This means that the transplant was successful, the new liver is functioning, and the recipient has recovered without major complications.
The five-year survival rate after liver transplant surgeries is 78%. The ten-year survival rate is 65%. These survival rates vary depending on the patient’s age, general health status, and the underlying reason for the liver transplant. In some cases, the condition may recur, and the disease may persist.