What is MS (Multiple Sclerosis)?
Multiple sclerosis (MS) is a condition where the immune system attacks the protective sheath covering nerve fibers, causing communication problems between the brain and the rest of the body. This condition, also known as MS, can result in permanent damage and deterioration of the nerve fibers.
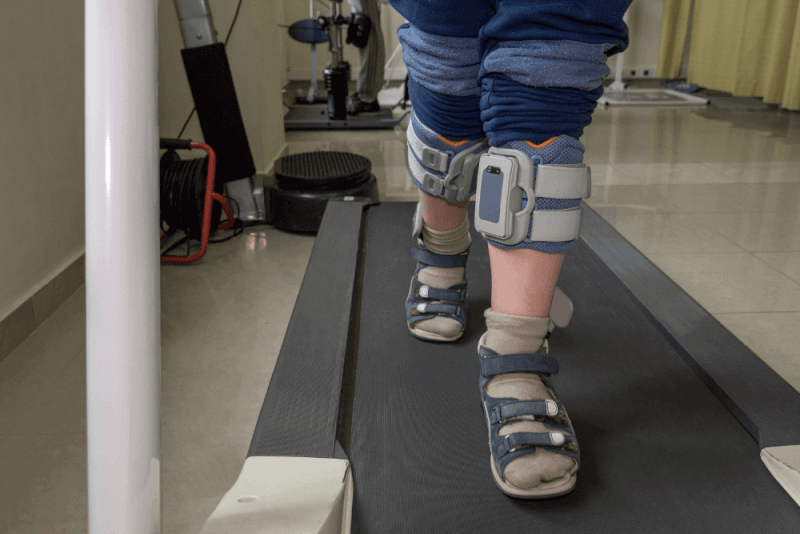
In severe cases of MS, patients may lose their ability to walk independently. Some MS patients may experience long-term remission without any new symptoms.
Although there is no cure for MS, treatment options are available to speed up recovery from attacks, modify the course of the disease, and manage symptoms.
Diagnosis Criteria for MS
There is no specific test for diagnosing MS. Diagnosis is made by excluding other conditions that may cause similar symptoms and considering the characteristic signs of MS.
First, a comprehensive medical history of the patient is taken, followed by a physical examination. Various tests may be applied to exclude other diseases.
- Blood tests to exclude other diseases with common symptoms of MS.
- A sample of cerebrospinal fluid is taken from the spinal canal to look for abnormalities in antibodies associated with MS. This sample also helps exclude infections and other conditions that cause symptoms similar to MS. A recently introduced new antibody test allows for faster testing of the sample.
- Magnetic resonance imaging (MRI) is used to reveal MS lesion areas in the brain and cervical and thoracic spinal cord. Intravenous contrast material may be injected to highlight lesions that indicate the disease is in an active stage.
- Evoked potential tests that record electrical signals produced by the nervous system in response to stimuli can be applied.
In most cases of relapsing-remitting MS, diagnosis is straightforward. Diagnosis is possible based on a series of symptoms consistent with the disease and brain imaging scans such as MRI.
However, diagnosing MS can be more challenging in people with unusual symptoms or progressive disease. In such cases, additional tests such as lumbar puncture and evoked potentials may be needed.
Symptoms of MS
Symptoms of MS vary depending on the location of the affected nerve fibers. Additionally, symptoms can vary significantly throughout the course of the disease, making diagnosis difficult. Common symptoms of MS include:
- Numbness and weakness in one or more limbs, typically on one side of the body at a time
- Tingling
- Electric shock sensations that occur with certain neck movements, especially when bending the neck forward
- Lack of coordination
- Unsteady gait
- Inability to walk
- Prolonged double vision
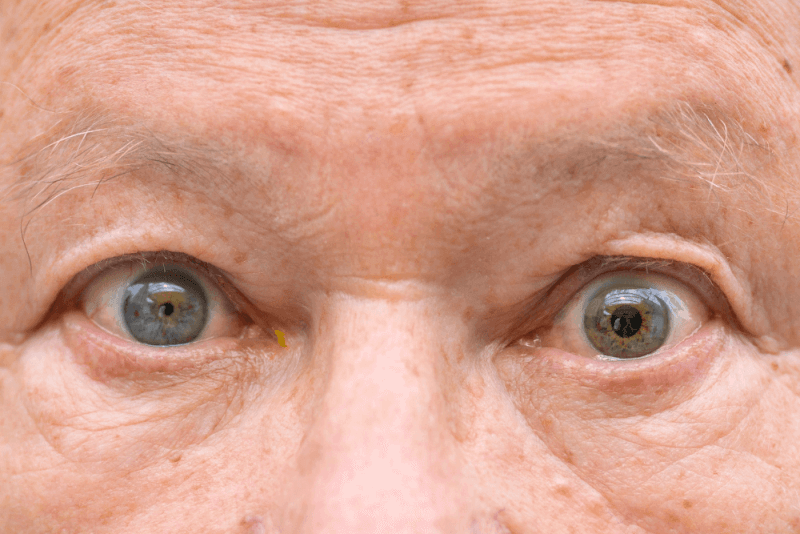
- Blurred vision
- Dizziness
- Bowel and bladder function problems
- Sexual problems
- Fatigue
- Speech problems
- Mood disorders
- Cognitive problems
Causes of MS
The cause of MS is unknown. MS is considered an immune-mediated disease because it results from the body's immune system attacking its tissues.
The immune system's attack on myelin can be compared to the insulation on electrical wires. When the protective myelin is damaged and the nerve fiber is exposed, the messages transmitted along the nerve fiber can be slowed or blocked.
It is unclear why some people develop MS while others do not. A combination of genetic and environmental factors is thought to be responsible for the condition.
Risk Factors for MS
The following factors increase the risk of developing MS:
- MS can occur at any age, but its onset is usually between 20 and 40 years old.
- Women are 2 to 3 times more likely to develop MS than men.
- The risk increases if a parent or sibling has MS.
- Infections caused by various viruses have been linked to MS.
- White people, especially those of Northern European descent, are at higher risk of developing MS. The risk is lower in people of African, Asian, or Native American descent.
- MS is more common in temperate climates.
- Low vitamin D levels increase the risk.
- Information on chromosome 6p21 has been found to be associated with MS.
- Obesity in women has been linked to an increased risk of developing MS.
- Having certain autoimmune diseases increases the risk of developing MS.
- Smoking increases the risk of developing MS.
Complications of MS
The following complications can occur in MS patients:
- Muscle stiffness and spasms
- Mood changes, such as depression and anxiety
- Severe weakness or paralysis, usually in the legs
- Memory problems
- Difficulty finding words
- Loss of bowel and bladder control
- Paralysis
- Sexual dysfunction
- Rarely, seizures
Treatment Methods for MS
There is no cure for MS. Treatment focuses on speeding recovery from attacks, reducing relapses, slowing disease progression, and managing MS symptoms. Some patients have very mild symptoms and do not require any treatment.
Treatments for MS Attacks
Treatment methods that can be applied to manage MS attacks include:
- Corticosteroids such as oral prednisone and intravenous methylprednisolone are prescribed to reduce nerve inflammation. Side effects of these drugs include increased blood sugar and blood pressure, insomnia, fluid retention, and mood changes.
- Plasma exchange involves taking a portion of the patient's blood, separating the blood cells from the plasma, mixing the blood cells with a protein solution called albumin, and returning the blood cells to the patient. This treatment is used when symptoms are severe or do not respond to other treatments.
Treatments to Prevent Disease Progression
Medications used in these treatments are applied aggressively in the early stages of MS to reduce relapse rates and slow the formation of new lesions, thereby potentially reducing the risk of brain lesions and disability accumulation. However, many of these treatments carry significant health risks.
Therefore, before deciding on these treatments, it is essential to carefully evaluate the duration and severity of the disease, previous MS treatments, other health problems, and factors such as childbirth. Treatment options to prevent disease progression include injectable, oral, and infusion medications.
Injectable Treatments Include:
- The most commonly prescribed medications for MS are interferon beta drugs. They work by fighting off immune cells that attack the body and can reduce inflammation and promote nerve growth. They are injected under the skin or into the muscle and can reduce the frequency and severity of relapses. Side effects of interferons include flu-like symptoms and injection site reactions. Additionally, blood tests are required to monitor liver enzymes. Some patients may develop neutralizing antibodies that reduce the effects of interferons.
- Glatiramer acetate is used to help prevent the immune system from attacking myelin. This drug, injected under the skin, may cause skin irritation at the injection site.
- Monoclonal antibodies, which target cells that damage the nervous system, are administered via subcutaneous injection. They help reduce brain lesions and worsening symptoms caused by MS. Possible side effects include infections, headaches, and reactions to the injection.
Oral Treatments Include:
- Teriflunomide, taken once a day, helps reduce relapse rates. Side effects include liver damage and hair loss. It is also associated with birth defects in both men and women, so birth control must be used while taking the drug and for two years after stopping it. Regular blood tests are also required to monitor the drug.
- Dimethyl fumarate, taken twice a day, is another drug used to reduce relapses. Side effects include flushing, diarrhea, nausea, and decreased white blood cell count. Therefore, the drug must be monitored with regular blood tests.
- Diroximel fumarate, also taken twice a day, is similar to dimethyl fumarate but causes fewer side effects. It is among the drugs approved for treating relapsing forms of MS.
- Delayed-release monomethyl fumarate has a slow and steady effect. Due to its timed release, side effects are expected to be reduced. Possible side effects include liver damage, flushing, abdominal pain, and infections.
- Fingolimod, taken twice daily, helps reduce relapse rates. However, it can slow the heart rate, so heart rate and blood pressure must be monitored for 6 hours after the first dose. Other side effects include reversible but rare serious infections, high blood pressure, and blurred vision.
- Siponimod, taken once a day, helps reduce relapses and may slow disease progression. It is also among the drugs approved for secondary progressive MS. Possible side effects include liver problems, viral infections, and low white blood cell counts. Other side effects include changes in heart rate, headaches, and vision problems. This drug can harm a developing fetus, so women who can become pregnant should use birth control while taking the drug and for 10 days after stopping it. Some patients may need to monitor their heart rate and blood pressure for 6 hours after the first dose. It is among the drugs that require regular blood tests for monitoring.
- Ozanimod, taken once a day, helps reduce relapse rates. Possible side effects include high blood pressure, liver inflammation, and infections.
- Ponesimod, taken once a day with an increasing dosage schedule, has a low relapse rate and has shown fewer brain lesions compared to some other MS medications. Side effects include respiratory tract infections, liver irritation, high blood pressure, and electrical problems in the heart affecting heart rate and rhythm.
- Cladribine, prescribed as a second-line treatment for relapsing-remitting MS, is also approved for secondary progressive MS. It is administered as two treatment courses over two weeks in a two-year period. Side effects include upper respiratory tract infections, tumors, headaches, serious infections, and decreased white blood cell count. People with active chronic infections or cancer, pregnant or breastfeeding women should not use this drug. Men and women must use birth control while taking the drug and for 6 months after stopping it.
Infusion Treatments for MS Include:
- Natalizumab, a monoclonal antibody, is used because it reduces relapse rates and slows disability progression. This drug is designed to keep potential immune cells that damage the nerves in the brain and spinal cord out of the bloodstream. It is a first-line treatment for severe MS patients and a second-line treatment for some severe MS patients. PML JC, a positive antibody for the agent, increases the risk of progressive multifocal leukoencephalopathy, a potentially severe viral brain infection. The risk of PML is very low in people without this antibody.
- Ocrelizumab, which slows the progression of primary progressive MS, is the only DMT approved by the FDA to treat both relapsing and primary progressive forms. Studies have shown that it reduces relapse rates and slows the worsening of disability in both forms of the disease. Side effects include injection site irritation, fever, low blood pressure, and nausea. Some people, including those with hepatitis B infection, cannot use this drug. The use of the drug increases the risk of certain types of cancer.
- Alemtuzumab, a monoclonal antibody that targets a protein on the surface of immune cells, reduces relapse rates and shows MRI benefits. This drug limits potential nerve damage caused by white blood cells. However, it increases the risk of severe thyroid autoimmune diseases and rare immune-mediated kidney diseases. The drug is given as an infusion over five consecutive days, then a year later, three additional days of doses. The drug is available only from registered providers, and the patient must enroll in a drug safety monitoring program when the drug is administered. This drug is typically used as a second-line treatment for aggressive MS patients or those who have failed other MS medications.
Treatments for MS Symptoms
Treatments that can be applied to reduce the severity of symptoms in patients include:
- Physical therapy helps increase muscle flexibility and strength, making it easier for patients to perform daily tasks. During therapy, patients are also taught how to use devices that facilitate the performance of daily tasks. Physical therapy and the use of mobility aids, if needed, help manage leg weakness and other functional problems caused by MS.
- Various muscle relaxants are used to reduce painful or uncontrollable muscle stiffness or spasms, especially in the legs.
- Various medications are used to reduce fatigue associated with the disease. However, these medications have not been proven to be superior to placebo and have been shown to cause more frequent side effects. Some antidepressants, including selective serotonin reuptake inhibitors, are used for this purpose.
- Medications used to increase walking speed can help patients slightly increase their walking speed. Side effects of these medications include urinary tract infections, insomnia, vertigo, and headaches. People with a history of seizures or kidney dysfunction should not use the medication.
- Various medications may be prescribed to control problems such as depression, pain, sexual dysfunction, insomnia, and bladder or bowel control associated with MS.
Nutrition in MS
Diet is very important in MS. In addition to healthy eating, lifestyle factors such as exercise and smoking affect the risk of developing MS and its progression. A healthy diet has a positive impact on MS for many reasons. Eating a healthy diet helps reduce relapses and the risk of disability.
Additionally, a healthy diet positively affects the bacteria living in the intestines, which has significant effects on the immune system that may be related to MS. However, there is no specific diet for MS patients. Instead, patients should generally adopt a healthy diet. Points to consider in nutrition include:
- Preparing meals at home as much as possible
- Eating colorful fresh fruits and vegetables every day
- Choosing lean protein sources
- Choosing healthy fats
- Choosing whole grains instead of refined grains
- Adding various herbs and spices to meals
- Limiting processed foods and added sugars
Types of MS
There are four common types of MS. These types should be seen as a way for doctors to describe symptoms.
Benign MS
Also called clinically isolated syndrome, benign MS involves the first attack of symptoms suggestive of MS, but MS criteria are not met. Inflammation and nerve damage cause symptoms. CIS can progress to MS.
Relapsing-Remitting MS
Relapsing-remitting MS, the most common form of MS onset, affects 85% of patients. This type of MS involves flare-ups of symptoms followed by remission periods.
Secondary Progressive MS
A significant portion of relapsing-remitting MS cases eventually progress to secondary progressive MS. In this type, nerve damage accumulates, and symptoms gradually worsen. Patients may still experience some relapses or flare-ups, but the likelihood of remission periods decreases.
Primary Progressive MS
In some patients, symptoms gradually start and worsen over time without any distinct relapses or remission periods. This condition is called primary progressive MS.
There are three rare variants of MS among these types:
Marburg Type MS
This variant is a very rare and rapidly progressing aggressive form. If left untreated, it can be fatal.
Tumefactive MS
In this variant of MS, demyelinations appear in the brain that can resemble tumors. In most cases, a brain tissue sample is needed to differentiate it from brain cancer and other problems.
Balo's Concentric Sclerosis
The most notable feature of this variant of MS is the presence of lesions with concentric rings of myelin damage on magnetic resonance imaging, which gives the condition its name.