30-Second Summary
- Raynaud’s Disease is a condition affecting small blood vessels in the fingers and toes, but it also affects blood vessels in the lips, earlobes, and nose.
- During a Raynaud attack, the arteries and capillaries in the fingers and toes become overly constricted. As a result, the skin in the affected area turns white and later blue.
- The secondary type generally appears in the 40s.
- Diagnosis of Raynaud's syndrome primarily begins with reviewing symptoms and medical history, followed by a physical examination.
What is Raynaud’s Syndrome?
Raynaud’s Disease is a condition that affects small blood vessels in the fingers and toes, but it can also affect blood vessels in the lips, earlobes, and nose. Raynaud's disease leads to episodic spasms called vasospastic attacks in response to cold, stress, and temperature changes.
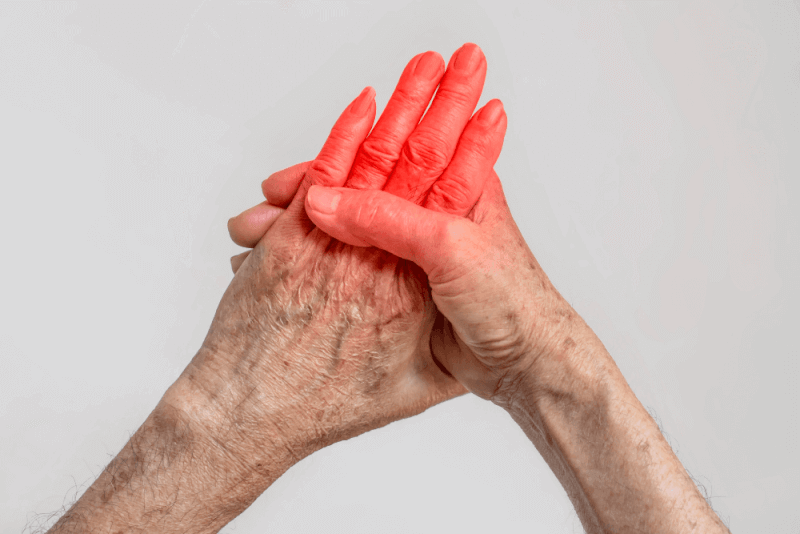
During a Raynaud attack, the arteries and capillaries in the fingers and toes constrict more than they should. As a result, the skin in the affected area turns white and later blue. This color change is due to a lack of oxygen in the blood. When the blood vessels relax and open, the skin turns red, and a tingling sensation may occur. Attacks typically last around 15 minutes.
Types of Raynaud’s Syndrome
Raynaud’s Syndrome has two different types:
Primary Raynaud’s Syndrome
The cause of primary Raynaud’s syndrome is unknown, and it is not associated with any other underlying condition. Symptoms in this type are generally mild, and no occurrences of skin cancer or gangrene are seen. The primary form is more commonly observed and can be treated with lifestyle changes. It is also referred to as Raynaud’s disease.
Secondary Raynaud’s Syndrome
Secondary Raynaud’s syndrome occurs due to an underlying disease or medication use. Symptoms can range from mild to severe, and skin ulcers or gangrene may develop. It is less common than primary Raynaud’s, but treatment requires addressing the underlying disease or discontinuing the causative medication. The term Raynaud’s phenomenon can also be used for secondary Raynaud’s disease.
Causes of Raynaud’s Syndrome
The causes of Raynaud’s syndrome vary based on the type of condition:
Causes of Primary Raynaud’s Syndrome
The cause of this common form is unknown. In many cases, the symptoms are so mild that they go unnoticed and resolve on their own over time.
Causes of Secondary Raynaud’s Syndrome
Secondary Raynaud’s phenomenon is caused by another underlying health condition. Though less common, it can lead to more severe clinical conditions due to more intense symptoms. Secondary Raynaud’s disease typically appears in the 40s. Causes include:
Connective Tissue Diseases
Scleroderma, a rare disease that causes the skin to harden and form scars, is commonly seen in individuals with Raynaud’s Disease.
Arterial Diseases
This includes conditions where fatty deposits build up in the arteries supplying the heart, as well as inflammatory conditions affecting blood vessels in the hands and feet. A type of hypertension that affects the pulmonary arteries also leads to Raynaud’s syndrome.
Carpal Tunnel Syndrome
Carpal tunnel syndrome, caused by pressure on the major nerves leading to the hands, results in numbness and pain, making the hands more sensitive to cold and hot temperatures.
Repetitive Movements or Vibration
Long periods of writing, playing the piano, or engaging in similar activities, as well as using vibrating tools like drills, can cause injuries that contribute to Raynaud’s disease.
Tobacco Use
Tobacco products negatively affect blood vessels and can cause Raynaud’s phenomenon.
Certain Medications
Medications that can cause Raynaud’s syndrome include certain blood pressure beta-blockers, some migraine medications, ADHD medications, some cancer treatments, and certain cold medications.
Symptoms of Raynaud’s Phenomenon
Symptoms that can occur due to Raynaud’s syndrome include:
Color Changes
When blood flow stops and then resumes, the skin color may change from white to blue and eventually to red. Not all patients experience all these color changes.
Cold or Numbness
When the fingers or other affected body parts do not receive oxygen-rich blood, numbness is a common sensation.
Warmth, Tingling, and Throbbing
This happens when blood flow returns to the affected area.
Skin Ulcers or Gangrene
Frequent or prolonged attacks can lead to painful sores on the fingertips. Healing of these sores can take time. In rare cases, tissue death can occur due to lack of oxygen.
Symptoms of Raynaud’s syndrome are episodic, meaning they come and go. Generally, attacks last about 15 minutes and are often triggered by cold weather.
Diagnosis Criteria for Raynaud’s Syndrome
Diagnosis of Raynaud’s syndrome starts with a review of symptoms and medical history, followed by a physical examination. Tests may be necessary to rule out other conditions with similar symptoms.
Tests
A test called nailfold capillaroscopy helps differentiate between primary and secondary Raynaud’s. During this test, experts use a microscope or magnifying tool to check for abnormalities in the skin beneath the nail, including swelling of blood vessels.
Blood tests help determine whether another condition, such as an autoimmune disease or connective tissue disorder, is causing the symptoms. These tests include:
- The antinuclear antibody (ANA) test, which checks if the immune system is attacking healthy tissues. This is called an autoimmune reaction, common in individuals with connective tissue or autoimmune diseases.
- The erythrocyte sedimentation rate measures how fast red blood cells fall to the bottom of a test tube. A faster rate may indicate inflammation or autoimmune disease.
No single blood test can diagnose Raynaud’s syndrome, but these tests can help detect associated conditions.
Treatment Methods for Raynaud’s Syndrome
Dressing in layers to protect against the cold is the first method often used to manage symptoms. Medications help control more severe symptoms. The goals of Raynaud’s syndrome treatment include:
- Reducing the frequency and severity of attacks
- Preventing tissue damage
- Treating the underlying disease or condition
Medications
Various medications may be used depending on the cause of symptoms. These include:
Calcium Channel Blockers
These medications help relax and open the small blood vessels in the hands and feet. They can also aid in healing wounds on the fingers and toes.
Vasodilators
These drugs help relax blood vessels. Some high blood pressure medications, erectile dysfunction drugs, antidepressant fluoxetine, and a class of drugs called prostaglandins are in this group.
Surgery and Medical Procedures
In cases of severe symptoms, surgery or injections may be necessary.
Neuro Surgery
The nerves in the hands and feet control the opening and closing of blood vessels in the skin. Cutting these nerves can stop these responses.
Small incisions in the affected hands and feet are made to strip small nerves around the supplying blood vessels. If the surgery is successful, the number and duration of attacks decrease.
Chemical Injection
Anesthetic drugs or botox injections can block the nerves in the affected hands and feet. In some cases, injections may need to be repeated if symptoms persist or return.
Lifestyle Changes
Lifestyle changes can reduce Raynaud’s syndrome attacks and help patients feel better. These changes include:
- Avoid smoking and second-hand smoke.
- Regular exercise increases blood flow and helps reduce symptoms.
- Stress management is important as stress triggers symptoms.
- Avoid rapid temperature changes.
Alternative Medicine
Practices and supplements that improve blood flow can help manage symptoms caused by the syndrome. However, it is important to consult a doctor about the effectiveness of these alternative treatments. Some alternative methods include:
- Fish oil helps increase blood flow.
- Ginkgo supplements help reduce the number of attacks.
- Acupuncture helps improve blood flow.
- Biofeedback is a method that allows the mind to control body temperature. This method involves exercises such as imagery, deep breathing, and relaxation to increase the temperature of the hands and feet.
Raynaud’s Syndrome Risk Factors
The risk factors for primary Raynaud's syndrome include:
- More common in women.
- Can occur at any age but is most commonly seen in individuals aged 15 to 30 years.
- More frequent in people living in cold climates.
- Having a parent or sibling with the disease increases the likelihood of developing it.
Risk factors for secondary Raynaud’s syndrome include:
- Some autoimmune diseases
- Use of vibrating tools or repetitive movements at work
- Smoking, medications that affect blood vessels, and exposure to chemicals like vinyl chloride.
What to do during Raynaud's syndrome attacks:
During attacks, hands and feet should be warmed up. Steps include:
- Move to a warmer environment.
- Move the fingers or toes.
- Place hands under your armpits.
- Draw large circles with your arms.
- Pour warm water on hands and feet.
- Massage hands and feet.
If the attack is triggered by stress, try to move away from the stressor and relax using a calming technique.
Triggers of Raynaud’s Syndrome
Triggers of Raynaud’s syndrome include:
- Cold areas such as air-conditioned rooms or frozen food sections in supermarkets.
- Anxiety, emotional stress, or excitement.
- Cold weather.
- Holding cold drinks.
- Reaching into a freezer.
- Sweating.