30-Second Summary
- Rheumatoid arthritis, one of the chronic diseases, is also classified as an autoimmune disorder.
- Uncontrolled inflammation damages the cartilage that acts as a shock absorber between joints. Over time, this leads to joint deformity and eventually bone erosion.
- The cause of this condition is not yet known. It is generally believed to result from a combination of genetic and environmental factors.
- Symptoms vary from person to person. However, fatigue is the most common complaint among patients and is considered the worst symptom of the disease.
What Is Rheumatoid Arthritis?
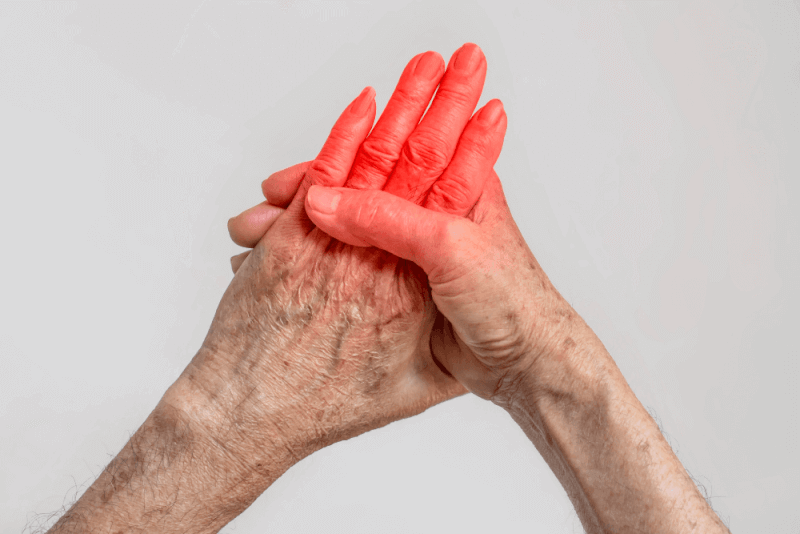
Rheumatoid arthritis, one of the chronic diseases, is also classified as an autoimmune disorder. It occurs in joints on both sides of the body, which distinguishes rheumatoid arthritis from other types of arthritis. Common sites of inflammation include:
- Fingers
- Hands
- Wrists
- Knees
- Ankles
- Feet
- Toes
Uncontrolled inflammation damages the cartilage that acts as a shock absorber between joints. Over time, this leads to joint deformity and eventually bone erosion. Bone erosion triggers the body's defense mechanisms, causing bones to fuse together for protection.
Certain cells in the immune system cause this process. The immune system substances produced in the joints circulate throughout the body and cause various symptoms. Therefore, in addition to the joints, rheumatoid arthritis can also affect the following tissues:
- Skin
- Eyes
- Mouth
- Lungs
- Heart
Causes of Rheumatoid Arthritis
Rheumatoid arthritis, one of the autoimmune diseases, occurs due to the immune system attacking the joints. However, the exact cause of this response is still unknown. It is generally thought to result from a combination of genetic and environmental factors.
Many different genes have been studied to understand the genetic link with rheumatoid arthritis. Some studies have found common genetic mutations, while others have not identified genetic factors.
In individuals with genetic factors, mutations in the human leukocyte antigen genes have been associated with a higher prevalence of rheumatoid arthritis. These genes help the immune system distinguish between the proteins of viruses and bacteria.
Symptoms of Rheumatoid Arthritis
Rheumatoid arthritis affects everyone differently. In some individuals, joint symptoms develop over several years, while in others they progress quickly. Many people experience a remission period following a flare-up when symptoms are not present.
Common symptoms of rheumatoid arthritis include:
- Pain, swelling, stiffness, and tenderness in multiple joints
- Stiffness in the morning or after long periods of sitting
- Pain and stiffness in the same joints on both sides of the body
- Fatigue
- Weakness
- Fever
- Loss of appetite
Symptoms vary from person to person, but the most common complaint among patients is fatigue. This is considered the worst symptom of the disease. Living with chronic pain can be very exhausting, and fatigue can make pain management more difficult.
Early-stage rheumatoid arthritis tends to affect small joints first, particularly those that connect the fingers to the hands and toes to the feet.
As the disease progresses, symptoms often spread to the wrists, knees, ankles, elbows, hips, and shoulders. In most cases, symptoms occur in the same joints on both sides of the body.
In addition, about 40% of patients experience symptoms that do not involve the joints. These include:
- Skin
- Eyes
- Lungs
- Heart
- Kidneys
- Salivary glands
- Nerve tissue
- Bone marrow
- Blood vessels
Rheumatoid Arthritis Flare-Up Symptoms
The symptoms of a rheumatoid arthritis flare-up are not different from regular symptoms. However, people with rheumatoid arthritis experience fluctuations in symptom severity. Flare-ups refer to more intense symptoms that appear after a period of feeling better. While treatment can lead to improved periods, changes in weather, certain foods, and infections can trigger the worsening of symptoms.
Rheumatoid Arthritis Diagnosis Criteria
To diagnose rheumatoid arthritis, doctors look for specific symptoms in patients. However, not all patients exhibit these symptoms. Diagnosis criteria include:
- Inflammatory arthritis in two or more large joints, such as shoulders, elbows, hips, knees, and ankles
- Inflammatory arthritis in small joints
- Positive biomarker tests such as rheumatoid factor or CCP antibodies
- Elevated CRP levels or sedimentation rate
- Symptoms lasting longer than six weeks
Diagnosing rheumatoid arthritis in its early stages is challenging because early symptoms can mimic those of other diseases. No single blood test or physical finding is definitive for the diagnosis.
During a physical exam, the doctor checks joints for swelling, redness, and warmth. Reflexes and muscle strength are also evaluated.
Blood Tests
Blood tests used in diagnosing rheumatoid arthritis include:
- Erythrocyte sedimentation rate (also called ESR)
- Elevated levels of C-reactive protein (CRP), which indicate the presence of inflammation in the body
- Rheumatoid factor
- Anti-cyclic citrullinated peptide (anti-CCP) antibodies
Imaging Tests
X-rays may be recommended to monitor the progression of rheumatoid arthritis in the joints over time. MRI and ultrasound tests can help doctors assess the severity of the disease in the body.
Rheumatoid Arthritis Treatment Methods
The goal of rheumatoid arthritis treatment is to reduce joint pain and swelling. This helps preserve and improve joint function. The long-term goal of treatment is to slow down or stop joint damage. Controlling joint inflammation reduces pain and improves quality of life.
Joint damage typically occurs within the first two years of diagnosis. Therefore, it is important to consult a doctor as soon as symptoms appear. This helps prevent long-term consequences of the disease.
Rheumatoid Arthritis Medication
The severity of symptoms caused by rheumatoid arthritis and how long the disease has been present determine the treatment. A single class of drugs or a combination may be prescribed.
NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Over-the-counter NSAIDs include ibuprofen and naproxen sodium. Stronger NSAIDs require a prescription. Side effects may include stomach irritation, heart problems, and kidney damage.
Steroids
Corticosteroids help reduce inflammation and pain and can slow joint damage. Side effects include bone thinning, weight gain, and diabetes. This drug class is often prescribed to quickly relieve symptoms and is tapered off gradually afterward.
Traditional DMARDs
These drugs slow the progression of rheumatoid arthritis. They help prevent joint and other tissue damage. Common DMARDs include methotrexate, leflunomide, hydroxychloroquine, and sulfasalazine. Side effects vary and may include liver damage and serious lung infections.
Biologic Agents
These newer drugs, called biologic response modifiers, are part of the DMARD class. They include abatacept, adalimumab, golimumab, infliximab, rituximab, sarilumab, and tocilizumab. Biologics are more effective when used in combination with traditional DMARDs. They may increase the risk of infections.
Targeted Synthetic DMARDs
When DMARDs and biologics fail to provide sufficient benefit, targeted synthetic DMARDs may be used. High doses of tofacitinib powders may increase the risk of blood clots in the lungs, serious heart issues, and cancer.
Rheumatoid Arthritis Physical Therapy
Physical therapy involving various exercises is used to help maintain joint flexibility. A therapist may also refer you to a physical or occupational therapist. Additionally, they can teach new ways to perform daily tasks to make joint movement easier.
Assistive devices can prevent strain on painful joints. Some aids can also help perform everyday activities more easily, such as dressing.
Rheumatoid Arthritis Surgery
If medications fail to prevent or slow joint damage, surgery may be considered to repair damaged joints. Surgery can restore joint function, reduce pain, and improve mobility.
Types of Rheumatoid Arthritis Surgery
Rheumatoid arthritis surgery may involve one or more of the following procedures.
Synovectomy
Surgical removal of the inflamed synovial membrane in the joint can help reduce pain and increase flexibility.
Tendon Repair
Inflammation and joint damage may cause tendons around the joint to loosen or rupture. The surgeon repairs these tendons.
Joint Fusion
Fusing a joint surgically can help realign or stabilize it and relieve pain when joint replacement is not an option.
Total Joint Replacement
During this surgery, the surgeon removes damaged parts of the joint and replaces them with a prosthesis made of metal or plastic.
Lifestyle Changes for Rheumatoid Arthritis
To relieve the symptoms of rheumatoid arthritis, patients need to make certain lifestyle changes in their daily lives. Combining these self-care recommendations with medications helps manage the symptoms.
Exercising Regularly
Light exercise can help strengthen the muscles around joints. It’s important to consult a doctor before starting. Those new to exercise should begin with walking. Avoid exercising joints that are tender, injured, or severely inflamed.
Applying Heat or Cold
Heat applications can relieve pain and help relax tense, aching muscles. Cold applications have a numbing effect and can help reduce swelling.
Relaxing
Finding ways to reduce life stress helps manage pain. Techniques like guided imagery, deep breathing, and muscle relaxation can all help control pain.
Alternative Medicine
Some popular complementary and alternative therapies show promise for rheumatoid arthritis. These include:
Fish Oil
Some preliminary studies suggest fish oil supplements may reduce rheumatoid arthritis pain and stiffness. Side effects may include nausea, burping, and a fishy taste. Fish oil can interact with other medications, so consult your doctor before use.
Herbal Oils
Evening primrose, borage, and black currant seed oils may help with rheumatoid arthritis pain and morning stiffness. Side effects include diarrhea and gas. Some herbal oils may cause liver damage.
Tai Chi
This movement therapy combines deep breathing with gentle exercises and stretches. Many use tai chi to reduce stress. These practices may improve mood and quality of life in people with rheumatoid arthritis. However, avoid movements that cause pain.
Rheumatoid Arthritis and Nutrition
Combining doctor-recommended treatments with dietary changes can help reduce inflammation and other symptoms of rheumatoid arthritis, but it does not cure the condition. It's important to add healthy fats to the diet while removing bad fats, salt, and processed foods. No dietary supplement, including collagen, can cure rheumatoid arthritis.
Losing weight may help relieve symptoms. Therefore, dietary changes that help achieve an ideal weight should be made. Additionally, individuals with rheumatoid arthritis are at increased risk for coronary artery disease. Thus, it’s recommended to add heart-healthy foods to the diet.
Stages of Rheumatoid Arthritis
Rheumatoid arthritis progresses in four stages. Each stage has its own treatment options.
Rheumatoid Arthritis Functional Loss
In the early stage, the joint lining or synovium becomes inflamed. Bones are not yet damaged, but the surrounding tissue usually swells, causing joint stiffness and pain.
Rheumatoid Arthritis Limited Disease
In this moderate stage, inflammation damages the cartilage, a cushion-like structure that protects the ends of bones. Joints become stiffer and lose mobility, resulting in limited range of motion.
Rheumatoid Arthritis Moderate Disease
In this severe stage, inflammation wears away both cartilage and nearby bones. Joints become unstable, and deformities start to appear as bones move. Pain, swelling, and loss of movement occur.
Rheumatoid Arthritis Severe Disease
In the final stage of rheumatoid arthritis, inflammation subsides, but damage continues. The joint stops functioning. Pain, swelling, stiffness, and lack of mobility are present. Joint replacement surgery is typically performed at this stage.
Rheumatoid Arthritis and Flare-Ups
Flare-ups can be short and sudden or severe enough to prevent patients from getting out of bed. During flare-ups, symptoms become significantly more intense.
Sometimes rest and self-care are enough during flare-ups. However, if symptoms worsen and flare-ups become frequent, the treatment plan should be reviewed.
General strategies during flare-ups include:
- Rest
- Relaxation
- Using assistive devices to support the joint
- Wearing proper footwear
- Engaging in light exercise
- Taking pain medications at the correct dose and on schedule
- Informing others about the flare-up
To manage pain, consider the following tips:
- Applying heat
- Applying cold
- Physical and mental relaxation
- Getting regular sleep
Rheumatoid Arthritis Risk Factors
There are several risk factors for developing rheumatoid arthritis. These include:
- Having a family history of rheumatoid arthritis
- Being female
- Smoking
- Obesity
Rheumatoid Arthritis Complications
People with rheumatoid arthritis are at higher risk for the following health conditions:
Osteoporosis
Both rheumatoid arthritis and medications used to treat the disease can weaken bones, making them more prone to fractures.
Rheumatoid Nodules
These firm tissue lumps typically form around pressure points like the elbows, but can also develop anywhere in the body, including the heart and lungs.
Dry Eyes and Mouth
Sjogren's syndrome, which causes dryness in the eyes and mouth, can occur alongside rheumatoid arthritis.
Infections
Both the disease and its treatment can make patients more susceptible to infections. Therefore, staying up to date with vaccinations is important.
Abnormal Body Composition
Even when patients have a normal weight, they may have more fat than lean mass.
Carpal Tunnel Syndrome
If the disease affects the wrists, inflammation can compress nerves in the hands and fingers.
Heart Problems
The disease can lead to hardened and clogged arteries, and may also cause inflammation of the sac around the heart.
Lung Disease
Patients are at increased risk for inflammation and scarring in lung tissue, which can cause progressive shortness of breath.
Lymphoma
Lymphoma, a type of cancer that affects the lymph system, is more common in people with rheumatoid arthritis.