What is vasculitis?
Vasculitis refers to the inflammation of blood vessels. This inflammation causes the walls of blood vessels to thicken, thereby reducing their width. Restricted blood flow can lead to organ and tissue damage. There are many types of vasculitis, though most are rare. Vasculitis can affect one or multiple organs and can be either short-term or long-term.
It can occur in people of all ages, but some types are more common in specific age groups. Depending on the type, it may resolve without treatment. However, many types of vasculitis require medication to control inflammation and prevent flare-ups. Being an autoimmune disease, vasculitis can also lead to serious complications like aneurysms.
Diagnosis of vasculitis
Diagnosis of vasculitis typically involves a physical examination and various tests. Additionally, it is important to know the symptoms the patient is experiencing and when they first appeared. Diagnosis often involves ruling out other conditions. Experts use several tests to determine the cause of the symptoms before diagnosing vasculitis. These tests include:
Blood tests
Blood tests check for signs of inflammation, such as high levels of C-reactive protein. A complete blood count (CBC) helps determine if there are enough red blood cells. Tests that look for specific antibodies, like the anti-neutrophil cytoplasmic antibody (ANCA) test, can aid in diagnosing vasculitis.
Imaging tests
Non-invasive imaging techniques help identify which blood vessels or organs are affected by vasculitis. These tests are also crucial for monitoring the response to treatment. Common imaging methods include computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET).
Angiography
During this procedure, a flexible catheter is inserted into a large artery or vein. A special dye is then injected into the catheter, and X-rays are taken as the dye fills the artery or vein. This allows doctors to see the outlines of all blood vessels.
Biopsy
A small tissue sample is taken from the affected area and examined in a laboratory. This helps to understand the damage caused by vasculitis.
Causes of vasculitis
Vasculitis, an autoimmune disease, occurs when the immune system attacks the blood vessels. The exact cause of this condition is unknown. However, certain health conditions that cause inflammation in the body can trigger vasculitis. In some cases, vasculitis can occur without any specific cause or trigger, known as idiopathic vasculitis. Triggers for vasculitis include:
- Certain types of cancer
- Infections
- Side effects of certain medications
- Other autoimmune diseases
- Infections such as hepatitis B and hepatitis C
- Blood cancers
Risk factors for vasculitis
Vasculitis can affect anyone, but certain disorders increase the risk. These risk factors include:
- Age
- Family history
- Lifestyle choices
- Medications
- Infections
- Immune system disorders
- Gender
What is cerebral vasculitis?
Also known as central nervous system vasculitis, this condition refers to inflammation of the walls of blood vessels in the brain and spinal cord. Various conditions and diseases can cause this inflammation. Although it is a serious condition, it is treatable. Factors that can cause central nervous system vasculitis include:
- Systemic lupus erythematosus
- Dermatomyositis
- Sarcoidosis
- Rheumatoid arthritis
- Viral or bacterial infections
- Systemic vasculitic disorders
Symptoms of cerebral vasculitis
Symptoms of vasculitis in the central nervous system can include:
- Seizures
- Encephalopathy
- Mood changes
- Personality changes
- Decreased level of consciousness
- Vision problems
- Weakness
- Forgetfulness
- Confusion
- Paralysis
- Transient ischemic attacks
- Prolonged severe headaches
- Sensory abnormalities
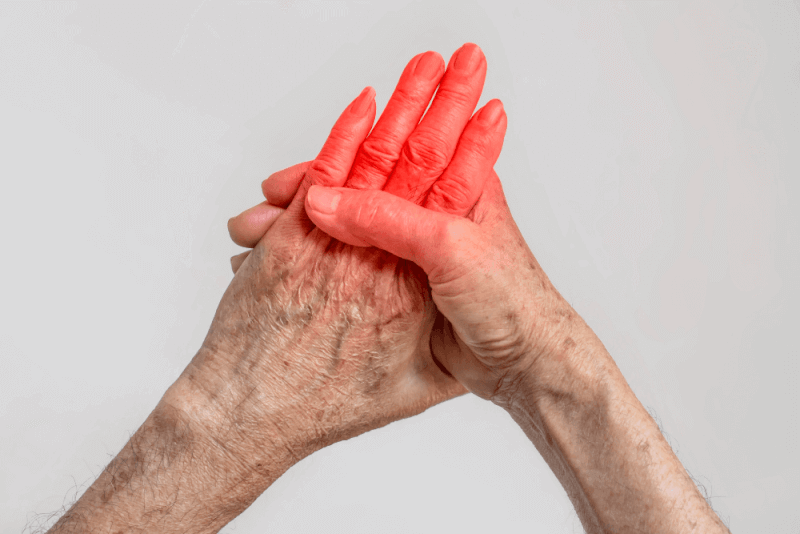
Symptoms of vasculitis
While symptoms of vasculitis vary depending on the type, general symptoms include:
- Fever
- General body aches
- Weight loss
- Fatigue
- Headache
Symptoms depending on the affected area may include:
- If the digestive system is affected, you may experience pain in the stomach and intestines after eating. Ulcers and perforations are possible, and there may be blood in the stool.
- If the ears are affected, you may experience tinnitus, dizziness, and sudden hearing loss.
- If the eyes are affected, you may experience itching, redness, or burning in the eyes. Giant cell arteritis can cause double vision or blindness in one or both eyes.
- If vasculitis affects the hands or feet, you may experience numbness and weakness. Additionally, the palms and soles may swell or harden.
- If vasculitis affects the lungs, you may develop shortness of breath and cough up blood.
- If the skin is affected, you may see red spots due to bleeding under the skin. Vasculitis can also cause swelling and open sores on the skin.
Treatment methods for vasculitis
Treatment for vasculitis focuses on controlling inflammation and managing underlying conditions.
Medications
Corticosteroid medications are used to control inflammation associated with vasculitis. However, long-term use of these drugs can cause serious side effects, including weight gain, diabetes, and weakened bones. When long-term treatment is necessary, the lowest possible dose of corticosteroids is used. Other medications are prescribed alongside corticosteroids to control inflammation. The specific medication depends on the type of vasculitis. These medications include:
- Methotrexate
- Azathioprine
- Mycophenolate
- Cyclophosphamide
- Tocilizumab
- Rituximab
Surgery
If vasculitis causes swelling or bulges in blood vessels, surgery may be needed to reduce the risk of rupture. Additionally, surgery may be required to open blocked arteries and restore blood flow to the affected area.
Types of vasculitis
There are many different subtypes of vasculitis. These subtypes are important for planning treatment and knowing the symptoms.
Behcet's disease
Behcet's disease is a rare condition that causes inflammation of blood vessels throughout the body. The disease can cause many symptoms that initially appear unrelated. Treatment aims to prevent serious complications such as blindness.
Symptoms of Behcet's disease vary among individuals and can come and go. In some people, the severity of symptoms decreases over time. The symptoms depend on the areas of the body affected. Commonly affected areas include:
- Mouth sores: The most common symptom of Behcet's disease, these sores start as raised, round lesions that turn into painful ulcers. Although they usually heal within 1 to 3 weeks, they may recur.
- Skin lesions: Some people develop acne-like sores on their bodies. These red, raised, and tender nodules usually develop on the lower legs.
- Genital sores: Red, open sores may develop on the scrotum or vulva. These sores are usually painful and leave scars after healing.
- Eye inflammation: Inflammation usually affects both eyes, causing redness, blurred vision, and pain. This condition can come and go.
- Joint swelling and pain: Usually affecting the knees, but also the ankles, elbows, or wrists. These symptoms can last for one to three weeks and may go away on their own.
- V ascular inflammation: Inflammation in veins or arteries can cause redness, swelling, and pain in the arms or legs. Inflammation in large arteries can lead to complications such as aneurysms and narrowing of blood vessels.
- Digestive symptoms: If the digestive system is affected, symptoms can include abdominal pain, diarrhea, and bleeding.
- Central nervous system: Inflammation in the brain and nervous system can cause headaches, fever, balance problems, weakness, and stroke.
Buerger's disease
Buerger's disease, also known as thromboangiitis obliterans, is a rare type of vasculitis that affects the arteries and veins in the arms and legs. It causes blood vessels to become inflamed, swollen, and blocked with blood clots, reducing blood flow. This can lead to damage and death of tissues in the affected areas, potentially resulting in gangrene.
This disease almost always occurs in people who use tobacco products. The only way to stop the disease is to quit using all forms of tobacco. In severe cases, amputation of affected fingers or toes may be necessary.
Symptoms of Buerger's disease include:
- Tingling or numbness in the hands or feet
- Inflamed veins just under the skin's surface
- Changes in skin color
- Painful open sores on the fingers and toes
- Fingers and toes turning white or blue in response to cold
- Pain in the feet or legs when walking
Churg-Strauss syndrome
Also known as eosinophilic granulomatosis with polyangiitis (EGPA), this type of vasculitis primarily causes adult-onset asthma. This disorder can also lead to other problems such as nasal allergies, sinus issues, skin rashes, gastrointestinal bleeding, and pain or numbness in the hands and feet. There is no cure for this rare type of vasculitis, but symptoms can be controlled with steroids and other powerful immunosuppressive drugs.
Symptoms of Churg-Strauss syndrome vary greatly among patients, with some experiencing mild symptoms and others facing severe, life-threatening complications. The disease typically progresses in three stages, each worsening over time. Almost all patients with this disease have asthma and an increased number of white blood cells. Other symptoms include:
- Loss of appetite
- Weight loss
- Joint pain
- Muscle pain
- Abdominal pain
- Gastrointestinal bleeding
- Weakness
- Fatigue
- General feeling of unwellness
- Rashes
- Skin sores
- Pain, numbness, and tingling in the hands and feet
Giant cell arteritis
This type of vasculitis involves inflammation of the lining of the arteries, usually in the temples. As a result, giant cell arteritis is sometimes called temporal arteritis. The aim of treatment, which involves corticosteroids, is to prevent vision loss.
Symptoms of giant cell arteritis include:
- Persistent severe headache, usually in the temples
- Fever
- Scalp tenderness
- Jaw pain when chewing or opening the mouth wide
- Vision loss or double vision
- Unintended weight loss
- Fatigue
- Sudden, permanent loss of vision in one eye
Kawasaki disease
This type of vasculitis causes inflammation in the walls of small to medium-sized blood vessels and can affect the coronary arteries that supply blood to the heart muscle. Kawasaki disease is also known as mucocutaneous lymph node syndrome because it also affects the lymph nodes, skin, and mucous membranes inside the mouth, nose, and throat.
Kawasaki disease primarily affects children under the age of 5. The disease is characterized by a high fever lasting more than five days and at least four of the following symptoms:
- Rash on the main body or genital area
- Swollen, red skin on the palms of the hands and soles of the feet
- Peeling skin on the fingers and toes
- Swollen lymph nodes in the neck
- Red, dry, cracked lips and a swollen, red tongue
- Red eyes without discharge
Symptoms of Kawasaki disease may not all appear at once. Therefore, if symptoms appear and then disappear, it is important to inform the doctor. Additional symptoms can include:
- Abdominal pain
- Vomiting
- Diarrhea
- Joint pain
In some cases, fever may persist for more than five days without the required four symptoms for diagnosing Kawasaki disease. This is known as incomplete Kawasaki disease. Even with fewer symptoms, children with incomplete Kawasaki disease still have a risk of heart damage and should be treated within 10 days of symptom onset. Kawasaki disease can cause symptoms similar to multisystem inflammatory syndrome in children (MIS-C), which has been seen in children with COVID-19.
Cryoglobulinemia
This type of vasculitis involves abnormal proteins called cryoglobulins that clump together at low temperatures. These clumps can block blood flow and damage skin, joints, nerves, and organs, especially the kidneys and liver. There are three types of cryoglobulinemia:
Type 1: Contains a single type of abnormal protein and is often associated with blood cancers. Type 2: Contains both monoclonal and polyclonal proteins and is often associated with hepatitis C virus. Type 3: Contains a mix of polyclonal proteins and is often associated with autoimmune diseases like rheumatoid arthritis.
Symptoms of cryoglobulinemia may not appear in some people, and when they do, they can come and go. Symptoms include:
- Purpura: Purple spots on the skin, particularly on the legs, that may look black or brown on darker skin. Some people may also develop ulcers, or open sores, on the legs.
- Arthritis-like joint pain is common.
- Peripheral neuropathy: Damage to the nerves in the fingers and toes, causing numbness and tingling.
Henoch-Schonlein purpura
Also known as IgA vasculitis, this type of vasculitis involves inflammation and bleeding in the small blood vessels of the skin, joints, intestines, and kidneys. The most striking feature of Henoch-Schonlein purpura is a purplish rash, typically on the lower legs and buttocks. Although it can affect anyone, it primarily occurs in children under the age of 10 and usually resolves on its own. However, if it affects the kidneys, medical attention is required.
Symptoms of Henoch-Schonlein purpura include:
- Purpura: Red or purple spots on the skin, often on the legs, buttocks, arms, face, and trunk.
- Rash can be more pronounced in areas of pressure, such as sock lines and waistbands.
- Joint pain and swelling, especially in the knees and ankles. Joint pain may occur one to two weeks before the rash appears.
- Abdominal pain
- Nausea
- Vomiting
- Bloody stools
- Nervous system symptoms, which often appear before the rash, may include headache, fever, balance problems, weakness, and stroke.
- If the kidneys are affected, there may be protein and blood in the urine.
Takayasu arteritis
Takayasu arteritis is a type of vasculitis that causes inflammation of the aorta and its main branches. Inflammation can lead to swelling, narrowing, or blockage of the arteries, which can cause tissue damage. The disease can progress without symptoms for years before it is diagnosed. Treatment aims to control inflammation and prevent further damage.
Symptoms of Takayasu arteritis include:
- Fatigue
- Unintended weight loss
- Muscle pain
- Joint pain
- Mild fever, sometimes accompanied by night sweats
- Weakness and pain in limbs with use
- Anemia
- Weak pulse
- Difficulty measuring blood pressure
- Differences in blood pressure between the arms
- Dizziness
- Fainting
- Headache
- Vision changes
- Memory problems
- Difficulty thinking
- Chest pain
- Shortness of breath
- High blood pressure
- Diarrhea
- Blood in the stool
Wegener's disease
Wegener's disease, also known as granulomatosis with polyangiitis (GPA), is a type of vasculitis that causes inflammation of the blood vessels in the nose, sinuses, throat, lungs, and kidneys. Early diagnosis and treatment can lead to full recovery. Without treatment, it can be fatal. Symptoms of Wegener's disease can develop suddenly or over several months. Early symptoms often affect the sinuses, throat, or lungs. Common symptoms include:
- Nasal crusting
- Nasal congestion
- Sinus infections and bloody or pus-like nasal discharge
- Fatigue
- Cough
- Bloody phlegm
- Fever
- Shortness of breath
- Wheezing
- Numbness in fingers or toes
- Blood in the urine
- Skin sores
- Bruising
- Rashes
- Eye redness, burning, pain, and vision problems
- Ear infections and hearing problems
Types of vasculitis
Vasculitis can be classified based on its cause and duration:
Acute vasculitis
Acute vasculitis refers to short-term inflammation of blood vessels.
Chronic vasculitis
Chronic vasculitis involves long-term inflammation of blood vessels, including conditions such as Behcet's disease and Takayasu arteritis.
Allergic vasculitis
Allergic vasculitis occurs as a reaction to medications and is characterized by inflammation of blood vessels.
Complications of vasculitis
Complications of vasculitis depend on the specific type and severity of the condition, as well as the side effects of medications used for treatment. Complications include:
- Organ damage
- Blood clots
- Aneurysms
- Vision loss
- Infections