30 Second Summary
- When kidney failure occurs, the kidneys cannot filter the blood as they should. As a result, waste and toxins accumulate in the bloodstream. Dialysis performs the kidney's function by removing waste products and excess fluid from the blood.
- Peritoneal dialysis involves small blood vessels in the abdominal membrane filtering the blood with the help of a dialysis solution.
- Hemodialysis can also be applied at home. Each session lasts a shorter time. For home hemodialysis, it must be done 4 to 7 times a week.
- Patients must track all the solid and liquid amounts they consume. In general, excessive fluid intake should be avoided. This helps control potassium, phosphorus, and sodium levels.
What is Dialysis?
Dialysis is used as a treatment when a person's kidneys completely lose their function. In kidney failure, the kidneys cannot filter the blood as they should. As a result, waste products and toxins accumulate in the blood. Dialysis takes over the kidney's role by cleaning the blood from these waste products and excess fluid.
Types of Dialysis
There are two main types of dialysis.
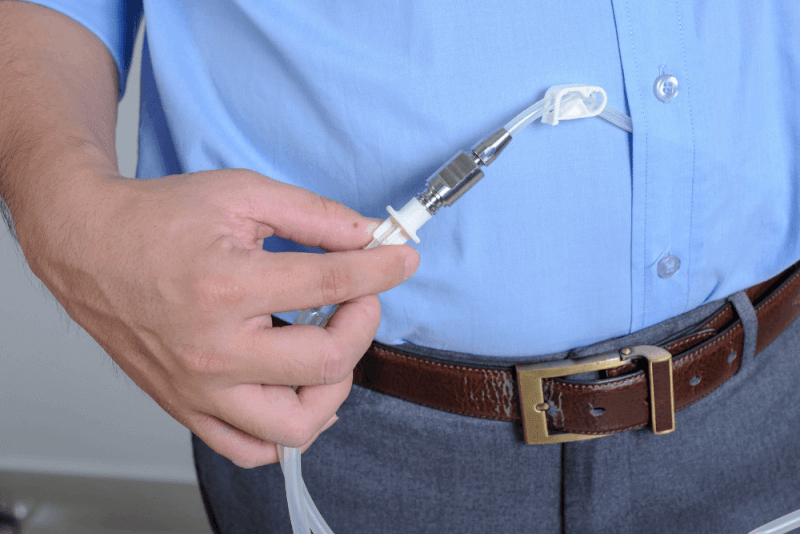
Peritoneal Dialysis
In peritoneal dialysis, small blood vessels in the abdominal membrane filter the blood with the help of a dialysis solution. This solution is a type of cleaning fluid containing water, salt, and other additives. Peritoneal dialysis can be performed at home. There are two methods of peritoneal dialysis. Automated peritoneal dialysis uses a machine called a cycler, while continuous ambulatory peritoneal dialysis is performed manually while standing.
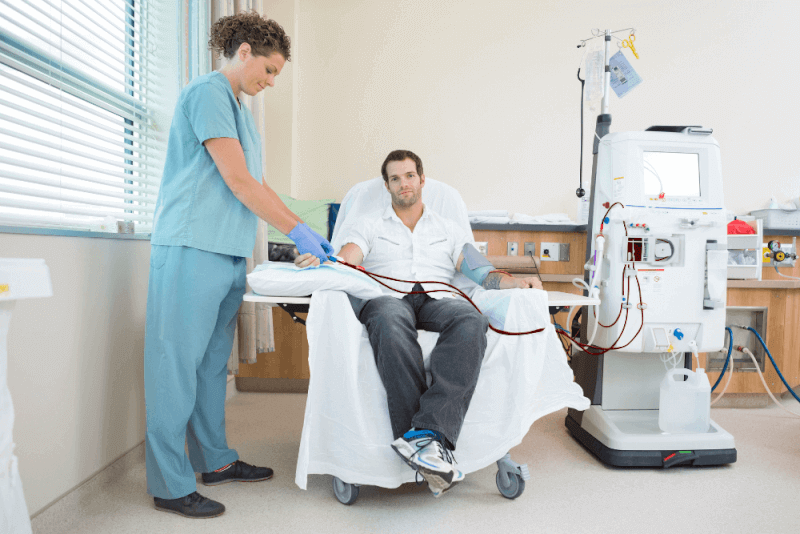
Hemodialysis
In this type of dialysis, a machine removes blood from the body, filters it through the dialyzer, and returns the cleaned blood to the body. The procedure typically takes 3 to 5 hours and must be done three times a week at a hospital or dialysis center.
Hemodialysis can also be done at home. Each session lasts for a shorter duration, and for home hemodialysis, it must be done 4 to 7 times a week. Most patients who perform home hemodialysis prefer to do it while sleeping at night.
The Dialysis Process
The dialysis process varies depending on the type of dialysis. Before starting dialysis, patients need to prepare.
Hemodialysis Process
Before hemodialysis begins, a small surgical procedure is performed to facilitate access to the bloodstream. This procedure involves creating two access points: the arteriovenous fistula (AV fistula) and the arteriovenous graft (AV graft). The AV fistula connects an artery and a vein, while the AV graft is used when the artery and vein are too short to connect directly.
The AV fistula and grafts widen the artery and vein, making dialysis access easier and helping blood flow more quickly. In emergency situations, doctors may place a catheter in the neck, chest, or leg for temporary access to the blood vessels.
The stages of hemodialysis are as follows:
- The dialysis machine draws blood from the needle in the arm.
- The blood circulates through the dialysis filter, where waste is transferred to the dialysis solution. The solution contains water, salt, and other additives.
- The filtered blood is returned to the body through another needle in the arm.
- Blood pressure is monitored to adjust the speed of blood flow into and out of the body.
Before starting peritoneal dialysis, a small surgical procedure is done to place a soft, thin catheter in the peritoneum (abdominal lining). This catheter is placed permanently. A healthcare provider teaches the patient how to perform peritoneal dialysis at home and how to protect the catheter from infection.
During peritoneal dialysis, the following happens:
- A Y-shaped tube is attached to the catheter. This tube connects to a bag containing the dialysis solution. The solution flows into the peritoneal space.
- After about 10 minutes, when the bag is emptied, the tube and catheter are removed.
- The catheter's cap is removed.
- The dialysis solution in the abdomen absorbs waste and excess fluid, while the patient can continue normal activities. This process takes 60 to 90 minutes.
- At the end of this period, the catheter cap is replaced, and the solution is drained into a clean, empty bag.
- This process can be repeated up to four times a day, and some patients choose to use the solution overnight.
Some patients prefer to perform peritoneal dialysis at night. In automated peritoneal dialysis, a machine called a cycler pumps the solution into and out of the body while the patient sleeps.
Conditions for Dialysis
Dialysis is used when the kidneys are no longer functioning properly. To start dialysis, kidney disease must be severe, and the kidneys can no longer filter waste and maintain the body's metabolic balance. Kidney failure can result from conditions like:
- Lupus
- High blood pressure
- Diabetes
- Injuries
In some cases, kidney disease can develop without any known cause. To begin dialysis, patients must show severe symptoms, and lab tests must indicate high levels of toxic waste in the blood.
Dialysis and Kidney Transplantation
For end-stage kidney disease, there are two options for treatment: dialysis and kidney transplantation. Dialysis does not cure kidney disease but helps manage symptoms. Kidney transplantation, on the other hand, provides a cure for kidney failure.
Although dialysis has seen improvements, mortality rates remain high. Kidney transplantation offers better outcomes, with higher survival rates and improved quality of life. Unlike dialysis, kidney transplant patients don't need significant changes to their diet.
What Happens If Dialysis is Not Performed?
The decision to stop dialysis is very difficult, especially for older patients or those in nursing homes. If dialysis is not started, or if a patient stops dialysis, they will likely die within a few weeks due to the buildup of toxins in the blood.
As toxins accumulate, physical and emotional changes occur. In the final stages, the body begins to shut down. Common symptoms in the last days include:
- Loss of appetite
- Sleeping most of the day
- Restlessness
- Seeing non-existent people
- Confusion
- Unable to recognize familiar faces
- Respiratory changes
- Congestion
- Changes in skin color and temperature
In the final stages, patients often choose not to eat or drink. They should not be forced to eat or drink, but if they wish, they can consume food or fluids.
Importance of Creatinine in Dialysis
It is normal to have a small amount of creatinine in the blood. Creatinine is filtered from the blood by the kidneys. When the kidneys aren't functioning properly, creatinine levels rise. Dialysis performs the same function, so creatinine levels are often checked to monitor how well dialysis is cleaning the blood.
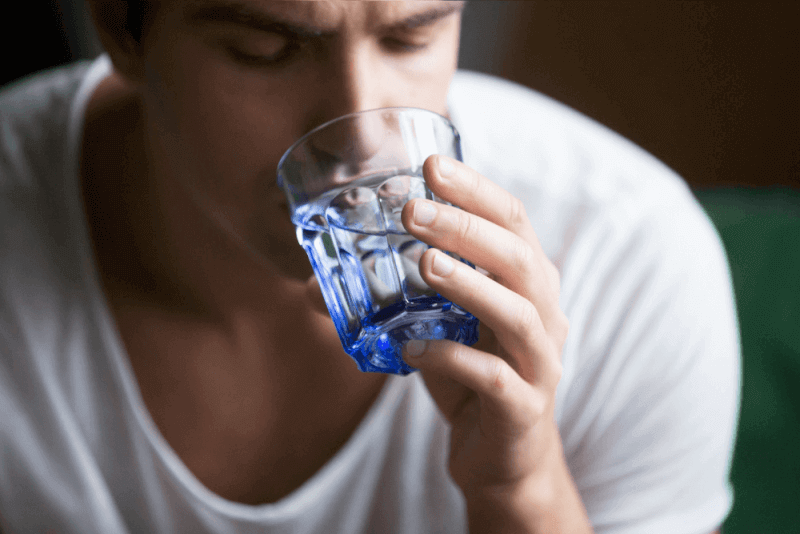
Nutrition for Dialysis Patients
The food and fluids consumed by dialysis patients can affect the efficiency of dialysis and how the patient feels. Improper nutrition can cause toxic buildup in the blood, making patients feel worse. Proper nutrition helps reduce toxin levels and improves well-being. Patients should monitor their fluid intake, as excessive fluid can lead to:
- Swelling and weight gain between dialysis sessions
- Blood pressure fluctuations
- Increased strain on the heart, leading to serious cardiac issues
- Fluid buildup in the lungs, making breathing difficult
Limiting sodium intake is crucial in managing fluid retention. High sodium levels cause thirst and increase fluid intake, which can be dangerous for dialysis patients.
Foods Considered as Liquids
The following foods are considered liquids:
- Soup
- Gelatin
- Pudding
- Foods with a lot of liquid in their recipe
- Melon
- Grapes
- Apple
- Orange
- Tomato
- Lettuce, celery
Potassium Intake
Potassium is vital for maintaining a steady heart rhythm, but excessive potassium can disrupt heart function, which is why dialysis patients must limit their intake.
Monitoring potassium intake is crucial to avoid dangerous heart problems, and patients should work with healthcare providers to ensure proper potassium levels.
Phosphorus Intake
Excessive phosphorus in the blood pulls calcium from the bones, weakening them and making them more prone to fractures. High phosphorus can also cause itchy skin.
Dialysis patients must limit phosphorus intake to protect their bones. Foods rich in phosphorus to avoid include:
- Processed foods
- Packaged foods
- Poultry
- Fish
- Nuts
- Peanut butter
- Beans
- Soda
- Tea, dairy products
Phosphate binders like sevelamer, calcium acetate, or calcium carbonate may be used to help manage phosphorus levels.
Protein Intake
Dialysis patients need to consume high-quality proteins, such as red meat, poultry, fish, and eggs, which produce fewer waste products.
Sodium Intake
Sodium, found in processed foods, canned foods, and fast food, should be limited to avoid excess thirst and fluid retention.
Calories
Many dialysis patients experience a loss of appetite. To ensure proper calorie intake, high-calorie foods like olive oil, rice, pasta, and bread should be added to their diet.
Butter and margarine should be avoided, as they are high in saturated fats that can cause plaque buildup in arteries, leading to blockages.
Patients who are overweight may need to reduce their calorie intake.
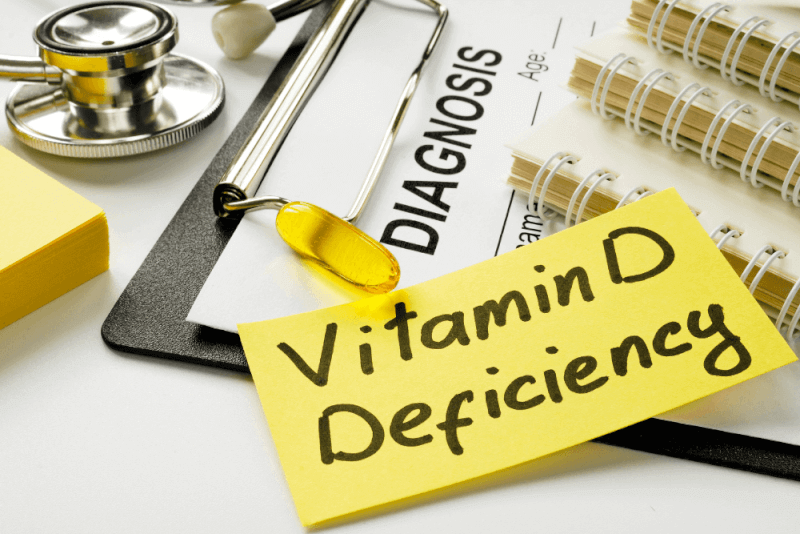
Vitamin and Mineral Supplements
Dialysis patients often experience vitamin and mineral deficiencies due to reduced intake and the loss of these nutrients during dialysis. Doctors will prescribe the necessary supplements, but patients should not take over-the-counter supplements without consulting their healthcare provider.
Side Effects of Dialysis
The side effects of dialysis depend on the type of dialysis performed. Common side effects of hemodialysis include:
- Low blood pressure
- Nausea
- Dizziness
- Fainting
- Chest or back pain
- Headache
- Itchy skin
- Muscle cramps
- Restless legs syndrome
In addition to these side effects, problems with AV fistulas or grafts can also arise. These problems may include:
- Infection
- Weak blood flow, scarring, or blockage due to clot formation
After peritoneal dialysis, some patients may experience bloating and a sensation of fullness. This is usually not painful, but it may cause discomfort due to the abdominal cavity being filled with fluid. Other side effects may include:
- Peritonitis, an infection caused by bacteria entering the abdominal cavity through the catheter
- Fever
- Abdominal pain
- Nausea
- Vomiting
- Weakening of abdominal muscles and hernia development due to the catheter use and fluid filling in the abdomen
- Accumulation of sugar (dextrose) from the dialysis solution, which may lead to weight gain over time