30-Second Summary
- Horner's Syndrome is a rare health condition affecting the surrounding tissues of one side of the eye or face. It occurs due to disruption in the sympathetic nerve pathway that connects the brainstem to the eyes and face. These nerves control involuntary functions such as sweating and pupil dilation.
- The types of Horner's Syndrome vary based on the patient's age and the location of the lesion. In 35-40% of cases, the type remains undetermined.
- The symptoms of Horner's Syndrome typically affect one side of the face.
- Specialists can diagnose Horner's Syndrome based on the patient's history and symptoms. Additionally, an ophthalmologist can confirm the diagnosis by administering medicated eye drops to both eyes.
What is Horner's Syndrome?
Also known as Bernard-Horner syndrome or oculosympathetic palsy, Horner's Syndrome is a rare health issue that impacts the surrounding tissues of one side of the eye or face. It arises due to damage to the sympathetic nerve pathway linking the brainstem to the eyes and face, which are responsible for controlling involuntary functions like sweating and pupil dilation.
Types of Horner's Syndrome
The types of Horner's Syndrome vary depending on the patient's age and the location of the lesion, with 35-40% of cases remaining undetermined.
Primary (Central) Horner's Syndrome
Also known as central Horner's syndrome or first-degree Horner's syndrome, Primary Horner's Syndrome involves processes such as hypothalamus, brainstem, and spinal cord lesions, demyelination, neoplasms, or syrinx.
This type of Horner's Syndrome extends caudally from the hypothalamus to the first synapse in the cervical spinal cord. The descending sympathetic pathway is in close proximity to other pathways and nuclei within the brainstem.
Pre-Ganglionic Horner's Syndrome
Also known as second-degree Horner's syndrome, pre-ganglionic Horner's syndrome originates in the spinal cord and progresses through the brachial plexus, the pulmonary apex, and synapses in the upper cervical ganglion within the cervical sympathetic chain. The upper cervical ganglion is located near the angle of the jaw and close to the bifurcation of the common carotid artery.
Post-Ganglionic Horner's Syndrome
The third-order neuron for the orbit enters the cranium through the adventitia of the internal carotid artery and into the cavernous sinus. Here, the oculosympathetic fibers emerge close to the trigeminal ganglion and the sixth cranial nerve, joining the first division of the trigeminal nerve before entering the orbit.
- These fibers innervate the dilator muscles of the iris and the smooth muscles of the upper and lower eyelids.
- Vasomotor and sudomotor fibers to the face ascend from the upper cervical ganglion along the external carotid artery.
- Pupil constriction is produced by parasympathetic fibers that accompany the third cranial nerve.
Causes of Horner's Syndrome
Horner's Syndrome occurs due to damage in the sympathetic nerve pathway, involving three different nerve cells. The causes vary depending on the type of nerve cells affected.
First-Order Neurons
This neuronal path begins in the hypothalamus at the base of the brain, passes through the brainstem, and extends to the upper part of the spinal cord. Issues in this area that could disrupt nerve function associated with Horner's syndrome include:
- Stroke
- Tumor
- Diseases causing loss of the protective sheath on neurons
- Neck trauma
- Cysts in the spine
- Sudden interruption of blood flow to the brainstem
- MS (Multiple Sclerosis)
- Chiari malformation
- Encephalitis
- Meningitis
Second-Order Neurons
This neuronal path extends in the spine from the upper chest to the side of the neck. Causes of nerve damage in this region include:
- Lung cancer
- Tumor of the myelin sheath
- Damage to the aorta exiting the heart
- Surgeries performed in the thoracic cavity
- Traumatic injuries
Third-Order Neurons
This neuronal pathway extends along the side of the neck to the skin of the face, the iris, and the muscles of the eyelids. Potential causes of damage in this area include:
- Damage to the carotid artery on the side of the neck
- Damage to the jugular vein on the side of the neck
- Tumors or infections near the base of the skull
- Migraines
- Cluster headaches
Children
The most common causes of Horner's Syndrome in children include:
- Injuries to the neck and shoulders during birth
- Congenital defects of the aorta present at birth
- Tumors affecting the hormonal and nervous systems
Symptoms of Horner's Syndrome
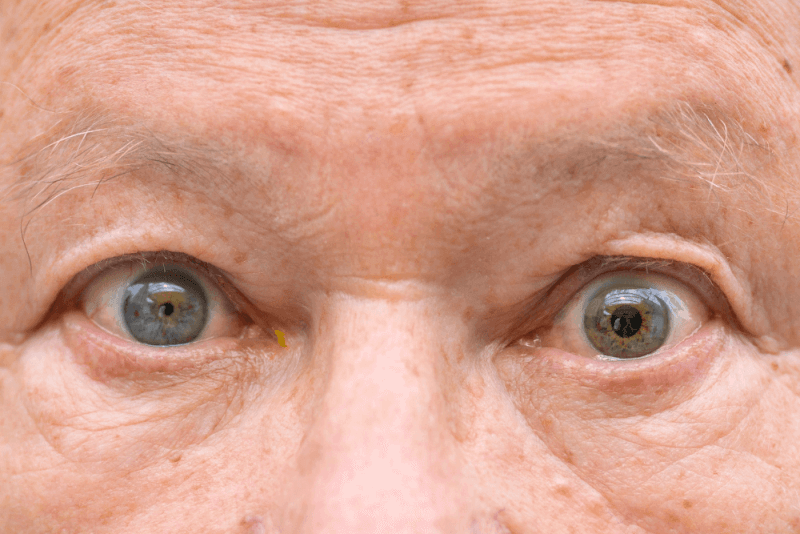
The symptoms of Horner's Syndrome generally cause one side of the face to be affected. Common symptoms include:
- A persistently small pupil
- A significant difference in pupil size between the two eyes
- Delayed or reduced pupil dilation in dim light on the affected side
- Drooping of the upper eyelid
- Slight elevation of the lower eyelid
- A sunken appearance of the affected eye
- Reduced or absent sweating on the affected side of the face
Symptoms related to sweating and the lower eyelid can be subtle, making diagnosis challenging.
Symptoms in Children
Potential symptoms of Horner's Syndrome in children include:
- A lighter iris color in one eye if affected before one year of age
- A change in color on the affected side of the face, often due to heat, physical exertion, or emotional responses
In addition to these symptoms, both adults and children can exhibit severe symptoms. Immediate medical attention is necessary if these symptoms appear, especially after trauma. These include:
- Vision problems
- Dizziness
- Speech difficulties
- Difficulty walking
- Muscle weakness
- Lack of muscle control
- Severe, sudden head or neck pain
Diagnostic Criteria for Horner's Syndrome
In diagnosing Horner's Syndrome, a physical examination is primarily conducted to assess the nature of the symptoms. Subsequently, various tests are performed to identify potential causes.
Tests to Confirm Horner's Syndrome
Experts can diagnose Horner's Syndrome based on the patient's history and symptoms. Additionally, an ophthalmologist can confirm the diagnosis by applying medicated eye drops to both eyes, which will cause pupil dilation or constriction in healthy eyes. This allows experts to compare the healthy eye with the eye that may have nerve damage.
Tests to Determine Nerve Damage
The characteristics of the symptoms help experts narrow down the cause of Horner's Syndrome. They may also perform additional tests or request imaging studies to locate the lesion or disorder disrupting the nerve pathway.
If the Horner's Syndrome is caused by a third-order neuron disorder, the doctor might apply a type of eye drop that significantly dilates the healthy eye and slightly dilates the affected eye.
To identify the potential location of the disorder causing Horner's Syndrome, the doctor may request one or several of the following tests:
- MR
- Magnetic Resonance Angiography for evaluating blood vessels
- Chest X-ray
- CT scan
Treatment Methods for Horner's Syndrome
There is no specific treatment for Horner's Syndrome itself. However, treating the underlying cause can resolve the syndrome. If the syndrome does not cause pain or any other discomfort to the patient, no treatment may be necessary.