30-Second Summary
- It is a condition where the amount of fat in the body is higher than normal. People with a body mass index (BMI) over 30 are considered obese.
- Symptoms include difficulty moving, back and joint pain, sleep apnea, increased sweating, general fatigue, and social isolation.
- Causes include overeating, a sedentary lifestyle, genetic factors, and hormonal disorders.
- Treatment options include diet, exercise, medication, and surgical interventions.
What is Obesity?
Obesity is a highly complex disease associated with having too much body fat. It is not merely a cosmetic concern but a medical condition that can lead to various health problems. Some of the most common medical issues include heart disease, diabetes, high blood pressure, high cholesterol, sleep apnea, liver disease, and certain types of cancer.
Some individuals may find it difficult to reach their ideal weight. Many different factors contribute to this condition. Obesity is often caused by a combination of hereditary, physiological, and environmental factors, along with poor diet, physical inactivity, and poor exercise choices.
The good news is that even a small amount of weight loss can help improve or prevent the health problems associated with obesity.
Causes of Obesity
The main cause of obesity is consuming more energy than the body can use. The reasons for consuming more calories than needed include the following:
Certain Medications
Some medications used to treat other health conditions can lead to weight gain. Examples include antidepressants, steroids, anti-seizure medications, diabetes medications, and beta-blockers.
Disability
Adults and children with physical and learning disabilities are at the highest risk for obesity. Physical limitations and a lack of proper education and resources can contribute to the problem.
Eating Habits
Consuming more calories than the body needs, highly processed foods, sugary foods and drinks, and foods high in saturated fat can lead to excess weight.
Genetics
Research on obesity has shown that some individuals with obesity may have genes that affect their appetite. However, it is unclear whether all overweight individuals share the same genetic makeup.
Lack of Physical Activity
Spending more time in front of a screen, such as watching TV or playing video games, reduces the time spent on physical activity. Less physical activity means the body burns fewer calories, which can lead to obesity.
Sleep Deprivation
Adults should sleep at least 7 hours per day. Sleeping less can disrupt hormones that control hunger, leading to weight gain.
Stress
The brain can respond to stress by producing more hormones, such as cortisol, which manage hunger. During stressful times, individuals are more likely to consume high-fat, sugary foods, which the body stores as extra fat.
Underlying Health Conditions
Conditions such as metabolic syndrome and polycystic ovary syndrome (PCOS) can lead to weight gain and other side effects. Mental health conditions like anxiety and depression may activate pleasure centers in the brain, leading to overeating high-calorie foods.
Risk Factors for Obesity
Factors that may increase the risk of developing obesity include:
- Genetics
- Poor lifestyle choices
- Certain diseases and medications
- Social and economic status
- Age
- Pregnancy
- Quitting smoking
- Sleep deprivation
- Stress
- Microbiome
Symptoms of Obesity
Although obesity is a disease, it does not cause specific symptoms. Healthcare professionals use the following measurements to identify obesity:
BMI Classifications
Doctors classify obesity based on BMI (Body Mass Index). There are three primary classes of obesity that doctors use to determine treatment methods for weight loss. These classes include:
- Class I obesity: A BMI between 30 and 35 or lower
- Class II obesity: A BMI between 35 and 40
- Class III obesity: A BMI over 40
It’s important to note that the BMI scale alone may not accurately predict certain health risks.
Waist Circumference
Where excess weight is stored on the body can indicate a higher risk of health problems caused by obesity. Women with a waist circumference greater than 89 cm and men with a waist circumference greater than 101 cm are at an increased risk for cardiovascular disease or type 2 diabetes.
Diagnostic Criteria for Obesity
In diagnosing obesity, a patient's height and weight measurements are taken, along with waist circumference. Tests such as bone density scans or bioelectrical impedance analysis may also be performed to assess body composition.
This test measures the body's composition based on the speed at which an electrical current passes through the body. The patient's general health is then assessed using additional diagnostic methods, which include:
- Questions regarding the patient’s medical condition, treatment history, and family health, including medications currently used
- Understanding previous weight management strategies and experiences
- Learning about current eating habits, sleep patterns, and daily activity levels
- Assessing factors that may impact stress and mental well-being
- Blood tests to monitor vital signs
Treatment Methods for Obesity
The primary goal of obesity treatment is to achieve and maintain a healthy weight. This improves overall health and reduces the risk of complications related to obesity.
It may be necessary to work with a team of healthcare professionals, such as a dietitian, behavioral counselor, or obesity specialist, to understand eating and activity habits and make the necessary changes.
The initial goal of obesity treatment is modest weight loss. This typically represents 5% to 10% of total body weight in obese individuals and 10% to 20% for those with extreme obesity.
All weight-loss programs involve changing eating habits and becoming more active. The right treatment methods for patients vary depending on their weight, general health, and willingness to participate in a weight-loss plan.
Diet Therapy
The key to obesity treatment is reducing calorie intake and adopting healthier eating habits. While rapid weight loss may be possible at first, long-term success depends on establishing consistent and healthy eating habits, which is the most reliable way to achieve sustained weight loss.
There is no one-size-fits-all weight-loss diet. However, patients must choose healthy foods and eat in appropriate portions. Diet changes in obesity treatment include:
Reducing Calorie Intake
To lose weight, calorie intake must be reduced. The first step is to review the number of calories typically consumed and their sources. This helps identify how many calories are consumed and where cuts can be made. Caloric needs vary, but basic calculations can determine patients' daily caloric requirements.
Gender, muscle mass, and daily activity levels should also be considered. Generally, women need between 1,200 and 1,500 calories per day, while men require between 1,500 and 1,800 calories per day.
Feeling Full with Less Food
Some foods, such as sweets, candy, fats, and processed foods, contain many calories in small portions. In contrast, fruits and vegetables contain fewer calories, allowing for larger portions. Eating larger portions of lower-calorie foods can reduce hunger and help consume fewer calories overall.
Making Healthier Choices
To improve the overall diet, it is recommended to consume more plant-based foods, including fruits, vegetables, and whole grains. Additionally, lean protein sources such as beans, lentils, soy, and lean meats should be included. It is also necessary to limit salt and added sugars. Reducing the amount of fat in the diet and choosing healthy fats is important as well.
Restricting Certain Foods
Some diets require the restriction of certain food groups, such as high-carbohydrate or full-fat foods. Health professionals will determine which diet plan is effective and which may be beneficial for the patient.
On the other hand, sugary drinks are generally high in calories, so limiting or completely removing them from the diet can be a great starting point for calorie reduction.
Meal Replacements
This type of diet plan involves replacing one or two meals with low-calorie shakes or meal bars and eating healthy snacks. Later, a healthy, low-fat, low-calorie meal is consumed. These diets can help with short-term weight loss. However, it can be difficult to turn them into a long-term lifestyle. Therefore, continuing the diet is necessary to help maintain weight loss.
The most important point to consider in diet therapy is to be cautious of quick fixes. It’s best to avoid the appeal of fad diets that promise rapid and easy weight loss. There are no magic foods or recipes for quick weight loss. Although fad diets may help with short-term weight loss, they often lead to worse results in the long term.
Similarly, crash diets can lead to weight loss, but there is a high likelihood of regaining the weight once the diet is stopped. Sustainable eating habits developed over time are necessary for both losing weight and maintaining the weight loss.
Exercise and Activity
Increasing daily physical activity is another crucial component of obesity treatment.
Exercise
Individuals undergoing obesity treatment should engage in at least 150 minutes of moderate-intensity physical activity per week. This helps prevent further weight gain or maintain moderate weight loss. As endurance and fitness improve, the amount of exercise may gradually increase.
Keep Moving
While regular aerobic exercise is the most effective way to lose weight, any extra movement throughout the day burns additional calories. Therefore, increasing daily physical activity is essential.
Behavioral Changes
Behavioral change programs are part of obesity treatment because they help with weight loss and maintaining weight loss. These programs assist with making lifestyle changes. Steps include examining current habits to understand which factors, stresses, or situations contributed to obesity.
Counseling
Meeting with a psychologist or psychiatrist can help address emotional eating behaviors. Therapy helps understand why overeating behaviors develop and teaches healthy ways to cope with anxiety. It also provides guidance on how to monitor diet and activity, recognize eating triggers, and manage food cravings. Counseling can be done one-on-one or in groups.
Support Groups
Support groups, where others share similar challenges with obesity, can offer friendship and understanding, making it easier to overcome difficulties.
Weight Loss Medications
There are medications available that can assist with weight loss. However, these medications must be used in conjunction with diet and exercise, as they are not effective on their own. Before deciding which medications to use, a patient's overall health and potential side effects must be considered.
Additionally, weight loss medications may not be beneficial for everyone. Over time, the amount of weight loss may slow down, and it is possible to regain the lost weight.
The active ingredients in commonly approved weight loss medications include:
- Bupropion-naltrexone, which can help reduce food intake
- GLP-1 agonists, which help control appetite, create a feeling of fullness, and lower blood sugar levels
- Semaglutide and tirzepatide, which suppress appetite and are often combined with GLP-1
- Liraglutide, which reduces appetite and slows digestion
- Orlistat, which reduces fat absorption in the intestines
- Phentermine-topiramate, which decreases appetite
- Phentermine, which reduces appetite but is only approved for 3-month use
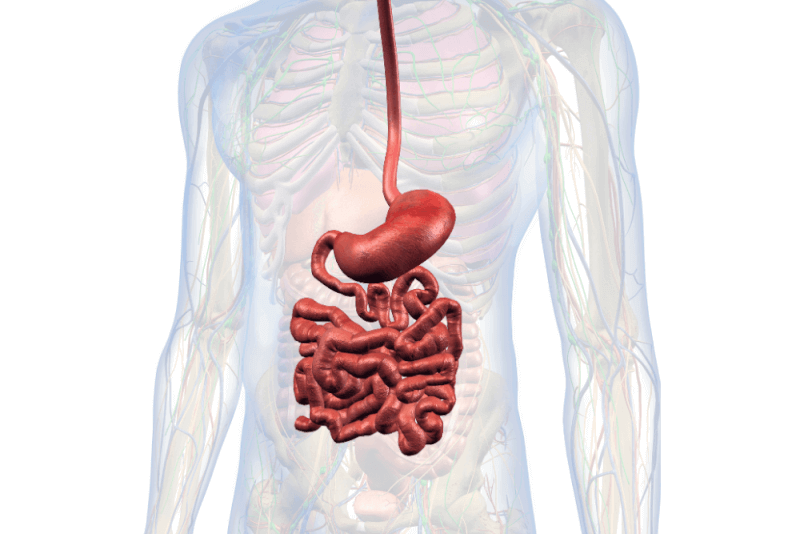
Obesity Surgery
Weight loss surgeries are generally recommended for patients with Class III obesity. Bariatric surgery typically involves altering parts of the stomach and small intestine. This reduces the amount of food that can be consumed, leading to reduced calorie intake. Some procedures also reduce hunger signals.
Types of Obesity Surgery
Obesity surgery is performed using various techniques, with some being more invasive than others. The most common types of obesity surgery include:
Duodenal Switch
The duodenal switch is a weight loss procedure that involves removing part of the stomach and bypassing the small intestine. This shortens the digestive path for food.
It also reduces the stomach’s capacity and affects how much is absorbed by the small intestine, making it a malabsorptive procedure. These changes also decrease hormones produced by the stomach and small intestine.
The duodenal switch is performed in two main ways: the original form, biliopancreatic diversion or gastric reduction with duodenal switch, and a newer version called loop duodenal switch, which simplifies the procedure and reduces complication risks.
While less common due to its complexity, the duodenal switch results in greater weight loss and longer-lasting outcomes compared to other procedures.
Gastric Band Surgery
Adjustable gastric band surgery involves surgically placing a device that restricts the amount of food the stomach can hold without permanently dividing the stomach. It is one of several obesity surgeries that help limit food intake.
Made of silicone, the inflatable band is placed around the upper part of the stomach and connected to a port under the skin for inflation. The surgeon injects saline into the device to tighten it, restricting the passage between the upper and lower parts of the stomach, creating a feeling of fullness with smaller amounts of food.
Gastric Bypass Surgery
Gastric bypass surgery is a metabolic and weight loss procedure that helps patients eat fewer calories and absorb fewer nutrients by altering both the stomach and the small intestine.
As with other bariatric surgeries, gastric bypass is recommended for patients with clinical obesity and can also help alleviate the following health issues:
- Type 2 diabetes
- Obstructive sleep apnea
- GERD
- Hyperglycemia
- Hyperlipidemia
- Hypertension
- Heart disease
- Fatty liver disease
- Osteoarthritis
Also known as Roux-en-Y, this procedure gets its name from the Y shape formed when the stomach and small intestine are divided and reconnected. The procedure creates a small stomach pouch, and part of the small intestine is rerouted to this new pouch, bypassing the rest of the stomach. The small intestine still functions to digest food, but the new route limits calorie intake and nutrient absorption.
Gastric Sleeve Surgery
Also known as gastric sleeve, this procedure reduces the size of the stomach, limiting calorie intake. About 80% of the stomach is removed, leaving it shaped like a tube.
This smaller stomach size reduces calorie intake and decreases the production of hunger hormones, allowing patients to feel full longer and lose weight more rapidly.
Benefits of Obesity Surgery
Different surgical methods are used in the treatment of obesity, and the benefits may vary depending on the chosen method. The potential benefits of each surgical procedure are as follows:
Duodenal Switch
Patients who undergo this procedure lose an average of 80% of their excess weight within 2 years. This rate is significantly higher compared to other obesity surgery methods. Additionally, patients can more easily maintain their ideal weight afterward. Studies show that 70% of patients continue to lose excess weight and maintain their weight 10 years post-surgery.
The success rate of this procedure is 90%, meaning that at least 90% of patients lose 50% of their excess weight. Furthermore, 90% of patients with Type 2 diabetes stop using medication after the surgery.
Other advantages of this method include:
- Improves metabolism, hunger, blood lipid levels, and blood sugar levels in the long term.
- Allows for slightly larger meal portions since more stomach tissue is left compared to other surgeries.
- Rarely causes dumping syndrome, meaning there is no need to avoid sugar or fat.
- Reduces the risk of death from any cause, allowing for a longer life.
Gastric Band
With gastric banding, patients can lose up to 40% of their weight. The results vary depending on how much patients change their habits after surgery.
The biggest advantage of gastric band surgery is that it has a lower risk of complications compared to other surgical methods and can be easily removed if necessary.
Gastric Bypass Surgery
The main advantage of gastric bypass is that it is the longest-established obesity surgery. Additionally, compared to other methods, it has one of the best long-term success rates.
Due to its long history, more data is available on this procedure. Studies show that patients can maintain their ideal weight even years after the procedure, and it improves other health conditions caused by obesity, reducing the need for medication.
Gastric Sleeve Surgery
Compared to other bariatric surgery procedures, gastric sleeve surgery is simpler, faster, and safer. It is the most suitable option for individuals with health conditions that are not appropriate for longer procedures. Since this method does not involve rearranging the intestines, the likelihood of long-term complications related to nutrition is much lower.
Complications of Obesity Surgery
Different methods used in obesity surgery can lead to different complication risks. Some complications are common across various procedures, but the severity and frequency of these common complications depend on the specific method. Possible complications for each procedure include:
Duodenal Switch
Common complications of this method, which can also be seen in other obesity surgery methods, include:
- Wound infections
- Excessive bleeding
- Reactions to anesthesia
- Blood clots
Procedure-specific complications for this surgery include:
- Hernias, where an organ pushes through an opening in the muscle wall.
- Intestinal obstruction due to scar tissue narrowing or compressing the small intestine.
- Anastomotic leakage, where the connection point in the bowel bypass leaks, potentially leading to a severe infection in the abdominal cavity.
Long-term complications of this procedure include:
- Malnutrition
- Diarrhea (this complication typically resolves as the digestive system adapts to the surgery).
- Bile reflux
- Gastritis and stomach ulcers due to bile reflux
- Gallstones
Gastric Band
The main disadvantage of the gastric band method is that it leads to less weight loss compared to other methods. Frequent adjustments are required during the first two years after surgery. Potential long-term issues include:
- The likelihood of complications after gastric band surgery is 50%.
- The rate of repeated procedures for inserting or removing the band is 35%.
- Additional interventions may lead to extra costs and risks.
Complications that may arise from gastric band surgery include:
- Nausea and vomiting are common, especially during the first days after surgery. This usually improves as patients learn how to eat properly.
- Constipation can occur due to difficulty in consuming sufficient fluids.
- Difficulty swallowing
- Reflux
- Port issues
- Outlet obstruction
- Band slippage
- Esophageal dilation and/or pouch enlargement
- Band erosion
- Band intolerance
Gastric Bypass
In the short term, the gastric bypass procedure shares similar risks with other procedures. However, complications specific to this procedure include:
- Hernia
- Small bowel obstruction
- Anastomotic leaks
Long-term complications of this method include:
- Dumping syndrome, where food moves too quickly from the stomach to the small intestine
- Malabsorption
- Nutritional deficiencies
- Bile reflux
- Gallstones
- Ulcers
- Weight regain
Gastric Sleeve
In addition to complications shared with other procedures, long-term complications of gastric sleeve surgery include:
- Scar tissue formed after surgery may cause narrowing of the stomach, slowing or blocking the passage of food, leading to nausea, vomiting, or difficulty eating.
- Nutritional deficiencies
- GERD
- Gallstones
Recovery After Obesity Surgery
The recovery process after obesity treatment varies depending on the chosen method. The recovery experiences associated with each procedure are as follows:
Duodenal Switch
After the surgery, patients are required to stay in the hospital for a few days. It takes a few weeks of rest before they can return to work or school. During recovery, significant changes occur in the body, including rapid weight loss. Some symptoms that may be experienced during this time include:
- Fatigue
- Nausea
- Hormonal fluctuations
- Mood swings
- Hair loss
- Body aches
- Chills
Additionally, there are strict dietary rules during recovery to allow the digestive system time to heal and adapt to the changes. Returning to a normal diet typically takes around 2 weeks. The recommended diets during this period include:
- Clear liquid diet
- Full liquid diet
- Pureed foods
- Soft diet
Gastric Band
Most patients lose weight within the first one to two years after surgery. Although the risk of immediate post-operative complications is rare, the risk of long-term complications is high. As a result, the band may need to be removed, followed by a bariatric procedure.
Gastric Bypass
After gastric bypass surgery, patients usually stay in the hospital for one day. They then rest at home for several weeks. For the first 6 weeks after surgery, patients should avoid strenuous activities, and it may take up to 12 weeks to return to normal activities.
Common symptoms during recovery include:
- Fatigue
- Mood swings
- Changes in bowel movements
Rapid weight loss and restricted eating during the first few months can lead to the following changes:
- Body aches
- Chills
- Hair loss
During recovery, patients must follow a strict dietary program. Following the diet closely helps protect the healing digestive system and promotes weight loss. In the first few weeks after surgery, a liquid diet is followed, then a soft diet, and finally, patients start consuming solid foods within two to three months. Special programs are created for each patient, but general recommendations include:
- Consuming two liters of fluids per day
- Consuming at least 100 grams of protein daily
- Taking daily vitamin and mineral supplements
- Avoiding foods high in sugar and starch
Gastric Sleeve Surgery
It takes about a month for patients to return to their routine after surgery. During this period, patients may feel tired as they adapt to a limited-calorie diet and recover. As with other procedures, patients start with a liquid diet, followed by soft foods, and eventually move to a specially planned solid food diet.
Endoscopic Procedures
Another method used in the treatment of obesity is endoscopic procedures. These procedures do not require any incisions. Instead, after the patient is under anesthesia, tubes and instruments are inserted through the throat into the stomach. Commonly performed procedures include:
Gastric Balloon
Gastric balloon is one of the most commonly used treatment options today. A small balloon is placed in the stomach, and it is filled with fluid to reduce the available space in the stomach, helping patients feel full faster with less food. The balloon remains in place for about six months and is then removed via endoscopy. If deemed appropriate by the healthcare team, a second balloon can be placed.
Endoscopic Sleeve Gastroplasty
In this procedure, stitches are placed in the stomach to reduce its capacity, which promotes weight loss by limiting food intake.
Hydrogels
These prescription capsules absorb water and expand in the stomach, helping patients feel full. They are taken before meals and are later excreted through the digestive system.
Vagus Nerve Blockade
In this method, a device is implanted under the skin near the stomach, which sends electrical signals to the vagus nerve. This nerve transmits signals to the brain about whether the stomach is full or empty.
Gastric Aspiration
In this obesity treatment method, a tube is placed in the stomach. After each meal, patients remove part of their stomach contents with the help of the tube.
What to Consider Before Obesity Surgery
Obesity surgery is a long-term treatment that affects patients' lives significantly. To achieve successful results, patients must do their part, and preparing for surgery is a key responsibility. Important points that patients need to consider before surgery include:
Learning to Eat
The key to weight loss surgery is for patients to learn healthy eating habits. Consulting a dietitian can provide detailed and professional guidance on pre-and post-operative diets.
Patients should also take vitamin and mineral supplements to meet their nutritional needs. If blood sugar regulation is necessary, an endocrinologist should be consulted for treatment.
Sticking to an Exercise Plan
In addition to surgery and diet, the healthcare team will prepare an exercise program for patients to promote weight loss. Patients should start following these lifestyle changes before surgery and commit to the exercise plan created by professionals.
Mental Health Assessment
Obesity surgery results in significant changes in patients' lives. Rapid weight loss also affects hormone levels, which can lead to mood swings. Mental health professionals should assess patients for any underlying issues, such as depression, and provide support. Therapy can help manage pre-and post-operative stress effectively.
Medical Clearance
Before surgery, patients' overall health must be evaluated, as these surgeries are complex. To reduce the risk of complications during or after surgery, lung function, metabolic status, and digestive system health should be checked.
Adopting Positive Behaviors
Before surgery, patients should adopt positive habits to support weight loss, including:
- Improving sleep habits
- Managing stress
- Seeking support from family, friends, or support groups
- Developing strategies to overcome emotional or social eating
- Quitting smoking
Anesthesia Preparation
Anesthesia presents risks even for healthy individuals, and these risks are higher for patients with obesity. Therefore, any factors that may affect anesthesia should be identified in advance, and the surgical plan should be adjusted accordingly.
What to Consider After Obesity Surgery
Obesity treatment can be challenging and lead to other health problems. After surgery, patients must continue their treatment thoroughly and make significant lifestyle changes, focusing on the following key areas:
Diet
After obesity surgery, healthcare professionals will create strict dietary programs for patients. In the first few weeks, these programs are usually very strict and mostly liquid. As patients continue to lose weight and maintain long-term results, they must follow a regular diet.
Post-surgery, fluid intake is particularly important. Consuming at least 2 liters of fluids per day helps alleviate nausea, kidney problems, fatigue, and constipation.
Meals should include high-protein foods, while starchy and sugary foods should be avoided.
Vitamins and Minerals
After obesity surgery, patients will need to take vitamin and mineral supplements for the rest of their lives. The supplements will be prescribed by their doctors and typically include vitamins B12 and D, as well as calcium and iron. Some patients may need to take chewable forms of supplements.
If supplements are not taken, patients may experience serious health issues due to deficiencies in vitamin and mineral levels.
Exercise
Exercise will help patients lose weight after surgery and maintain their weight in the long term. As patients feel more energetic after surgery, they will likely increase their exercise levels. Exercise programs start just a few hours after surgery, with patients encouraged to walk frequently. Professional guidance should be sought before starting an exercise program.
Patients are advised to exercise for at least 30 minutes a day after obesity surgery, with many patients naturally increasing their exercise duration over time.
Medications
Many patients are able to stop taking their pre-surgery medications after obesity surgery. Some medications, however, may need to be continued in liquid or chewable forms.
Patients who were taking extended-release medications before surgery may need to have their dosages adjusted. All medications should be taken under medical supervision.
Smoking and Alcohol
Before surgery, healthcare professionals recommend that patients quit smoking, which can be challenging. Doctors may prescribe treatments to help patients quit smoking, and other nicotine products should also be avoided.
Nicotine increases the risk of lung complications and impairs healing. Smoking increases the risk of pneumonia, blood clots, and heart attacks in patients who continue smoking before surgery.
Alcohol consumption after surgery can also lead to serious consequences, as alcohol is absorbed more quickly into the bloodstream post-surgery. This increases the risk of alcoholism compared to pre-surgery levels.
Pregnancy
Women should plan birth control methods before surgery, as it is recommended to avoid pregnancy for 12-18 months post-surgery. This allows patients to reach their ideal weight and ensure they can meet their and their baby's nutritional needs during pregnancy.
On the other hand, women who struggled with fertility before obesity surgery are more likely to conceive after the surgery. Even women who did not menstruate before reaching their ideal weight have been known to have healthy reproductive systems and become pregnant afterward.
Long-Term Follow-Up
Weight loss is a long-term process, and patients must be followed up after surgery. For the first few years after surgery, patients should visit their doctor once a month, as obesity is a chronic condition and can recur even after reaching the ideal weight.
Regular blood tests should also be conducted as part of long-term follow-up care. Blood tests should be performed at 3, 6, and 12 months after surgery, and then annually. Tests may include:
- Complete blood count (CBC)
- Comprehensive metabolic panel
- Lipid panel
- Hemoglobin A1c
- Vitamin and mineral levels
Obesity Recovery
Losing excess weight is a sign that the patient is in the recovery phase from obesity. Weight loss has a wide range of positive effects on patients' lives. Some of the benefits include:
Improved Sleep Quality
Obesity can cause sleep apnea, leading to poor sleep quality and chronic fatigue. However, weight loss helps improve breathing issues, allowing patients to enjoy more restful sleep and feel more energetic.
Better Mood
Weight loss improves not only physical health but also mental health, reducing symptoms of depression, anger, and tension.
Taste Changes
Obesity can dull taste buds, but patients often report improved taste after obesity surgery. Many develop aversions to sugary or fatty foods.
Brain Benefits
Obesity can negatively affect memory, thinking, and overall brain function. However, after weight loss, brain function improves, and studies show that certain areas of the brain become more active.
Improved Sexual Life
Many obese individuals have little interest in sexual activity, and obese men often suffer from erectile dysfunction. However, weight loss improves these issues, leading to a more satisfying sexual life.
Loose Skin
One of the rare side effects of weight loss is loose skin, especially in individuals who lose significant amounts of weight. This may require skin-tightening surgeries later, as loose skin can cause irritation and increase the risk of infection.
Slowed Metabolism
Another issue during recovery is a slowed metabolism. Consuming fewer calories causes the metabolism to slow down, which can hinder further weight loss. To overcome this, resistance exercises should be performed to increase muscle mass.
Body Clock Adjustment
The recovery process promotes a highly regulated lifestyle, resetting the body's internal clock. Additionally, meal timing plays a crucial role in weight loss, with some studies showing that meal timing can have positive or negative effects on weight loss.
Body Temperature Changes
Obese individuals tend to have higher body temperatures than others, particularly exacerbating symptoms during menopause. However, as weight loss progresses, body temperature returns to normal.
Obesity Risks
Individuals struggling with obesity are at higher risk of developing several potentially serious health conditions, including:
Heart Disease and Stroke
Obese individuals are at increased risk of heart disease and stroke due to high blood pressure and unhealthy cholesterol levels.
Type 2 Diabetes
Obesity affects the body's ability to use insulin to control blood sugar levels, leading to insulin resistance and an increased risk of diabetes.
Certain Types of Cancer
Obesity increases the risk of developing cancers such as uterine, cervical, endometrial, ovarian, breast, colon, rectal, esophageal, liver, gallbladder, pancreatic, kidney, and prostate cancer.
Digestive Problems
Obesity increases the likelihood of digestive problems such as heartburn, liver issues, and gallbladder disease.
Sleep Apnea
Obese individuals are at higher risk of developing sleep apnea.
Osteoarthritis
Obesity puts increased stress on the joints, encouraging inflammation, swelling, and pain, which can lead to complications such as osteoarthritis.
Fatty Liver Disease
Obesity can cause the accumulation of excess fat in the liver, leading to severe liver damage, including cirrhosis in some cases.
How Obesity Is Calculated
The first value used in diagnosing obesity is body mass index (BMI). To calculate BMI, divide the person's weight (in kilograms) by the square of their height (in meters). This calculation provides a rough estimate of obesity risk and body fat percentage.
BMI results are interpreted as follows:
- Below 18.5: Underweight
- 18.5 to 24.9: Healthy weight
- 25 to 29.9: Overweight
- 30 to 34.9: Class 1 Obesity
- 35 to 39.9: Class 2 Obesity
- 40 and above: Class 3 Obesity
Obesity Classifications
Obesity is classified based on BMI calculations and is generally divided into three classes. Some experts further subdivide Class 3 obesity into two additional subcategories:
- BMI between 50 and 59: Super Obesity
- BMI of 60 and above: Super-Super Obesity