30-Second Summary
- Overactive bladder is a condition characterized by a sudden urge to urinate and involuntary leakage.
- It can occur at any age, but it is more common in women and the elderly.
- Causes include aging, caffeine, alcohol, stress, and certain medications.
- Treatment options include lifestyle changes, medication, surgery, and other therapies.
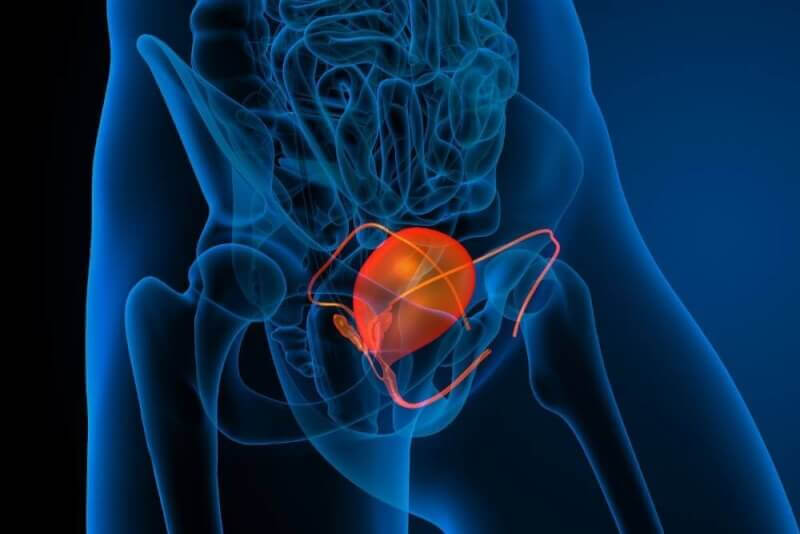
What is Overactive Bladder?
Also known as the hyperactive bladder, overactive bladder refers to a set of issues that arise when patients feel an urgent need to urinate. These issues do not include urine leakage or accidents.
Essentially, overactive bladder means patients frequently experience the urge to urinate. It is a condition caused by the activity of the muscle group responsible for emptying the bladder. Therefore, patients may feel the need to urinate even when the bladder is not fully full.
Symptoms of Overactive Bladder
Medically, the bladder should be emptied between 4 to 8 times a day. Patients who feel the urge to urinate more than eight times are considered to have an overactive bladder. The most commonly affected groups are women of all ages and the elderly.
Other symptoms of overactive bladder include bedwetting, not reaching the toilet in time, and more frequent nighttime urination. Urine leakage is not a symptom of overactive bladder. If patients experience this symptom, the issue is usually referred to as urge incontinence.
Who is Affected by Overactive Bladder?
Overactive bladder is generally prevalent across all age groups and races. However, it is most commonly seen in postmenopausal women and men with prostate conditions. On the other hand, children who are new to toilet training often experience overactive bladder as well.
How is Overactive Bladder Diagnosed?
The most critical factor in diagnosing overactive bladder is the patient’s history. Therefore, patients are often asked to keep a bladder diary to diagnose overactive bladder. The diary should include information such as the frequency of urination during the day and night, the comfort intervals between urinations, the presence of sudden urges, the ability to delay urination, the type of leakage, the use of pads, difficulty in urination, and any history of urinary retention. Additionally, patients should note any history of neurological diseases, vaginal or incontinence history, and radiotherapy.
Causes of Overactive Bladder
The causes of overactive bladder can be listed as follows:
- Cognitive decline due to aging
- Excessive consumption of alcohol, coffee, and carbonated beverages
- Diuretic medications
- Conditions that prevent the bladder from emptying
- Hormonal changes experienced by women during menopause
- Bladder muscle damage due to neurological diseases and treatments
- Diabetes
- Obesity
- Urinary tract infection
Treatment Methods for Overactive Bladder
There are many treatment options for overactive bladder. Determining which treatment to choose depends on identifying the underlying causes of overactive bladder.
Lifestyle Changes
The first step in treating overactive bladder is asking patients to change their lifestyles if necessary. These changes include maintaining an ideal weight, reducing caffeine intake, consuming fiber-rich foods to alleviate constipation, reducing excessive fluid intake, cutting down on carbonated drinks, and quitting smoking.
Pelvic Floor Muscle Training
Pelvic floor muscle exercises can help control the muscles that manage the bladder. For this reason, Kegel exercises and biofeedback are often recommended to patients.
Behavioral Therapies
Another treatment method used for overactive bladder is behavioral training. This training is divided into three types: bladder training, timed voiding, and habit training.
Electrical Stimulation
One of the treatments that need to be applied daily, electrical stimulation involves a minimum of two years of treatment. Probes placed in the vagina deliver electrical stimulation to the pelvic floor muscles.
Electromagnetic Therapy
Electromagnetic therapy works on the same principle as electrical stimulation. However, in this treatment method, the pelvic muscles and sacral roots are stimulated without using a probe. Although the exact mechanism of action is not fully understood, passive pelvic floor exercises can help control the hyperactivity of the muscles that manage the bladder. The main downside of this treatment is that it requires repeated sessions in a clinical setting.
Pharmacological Treatment
Some medications are also used to control the involuntary contractions of the bladder muscles. The most commonly used drug group in this context is anticholinergics. These drugs block the factors that cause bladder muscle stimulation. The first effects are typically seen within two weeks.
The effectiveness and side effects of these medications vary among patients. In overactive bladder cases, medications can reduce incontinence rates by 70% to 75% and the frequency of urination by 20% to 30%, while increasing urine volume by 10% to 20%.
In addition, intravesical agents are available, although some of them are not yet used in our country. However, botulinum toxin, commonly known as Botox, is used particularly in patients with overactive bladder resistant to other treatments.
Sacral Neuromodulation
Sacral neuromodulation is one of the most expensive treatments for overactive bladder. It has been observed that 50% of the storage symptoms in 80% of patients improved with this method. The procedure involves placing an electrode at the sacral 3 (S3) level of the spinal medulla through an intervention. This electrode is continuously stimulated by a generator.
Augmentation Cystoplasty
Augmentation cystoplasty is the last resort in treating overactive bladder. This treatment is applied to patients who are resistant to other treatments and those with severe symptoms. The aim of this procedure is to create a high-functioning, low-pressure bladder. In this procedure, the bladder is divided into two parts, and an intestinal segment is inserted between them. This not only increases the bladder’s capacity but also acts as a buffer against involuntary contractions.
Overactive Bladder Exercises
Exercises designed to reduce incontinence in overactive bladder focus on strengthening the pelvic floor muscles. These muscles not only support the bladder but also the bowel and uterus. Exercises that can help strengthen the pelvic floor muscles include:
Kegel Exercises
Kegel exercises are the most effective exercises for men and women who cannot control their bladder. They also speed up recovery after childbirth or prostate surgery. The steps for Kegel exercises are as follows:
- First, the muscles used to stop the flow of urine should be identified. These are the muscles used to stop the flow of urine while urinating.
- Once identified, these muscles should be squeezed as tightly as possible.
- Hold the position for 5 seconds. Then, rest for a few seconds and repeat the exercise.
- Over time, the duration of muscle contraction should be increased.
Squat
Squats not only help with incontinence but also strengthen the hips, thighs, obliques, and hamstrings. Additionally, this exercise burns many calories, aiding in weight loss. The steps for this exercise are as follows:
- Stand with feet flat on the ground.
- Place your feet shoulder-width apart.
- Slowly bend your knees as you lower your hips towards the ground.
- Lean slightly forward while keeping your back straight.
- Then, slowly return to an upright position.
- Throughout the exercise, keep the pelvic floor muscles and glutes tight.
- Repeat the exercise 10 times.
Over time, the number of repetitions should be increased. Maintaining proper posture during the exercise is crucial to avoid knee pain.
Bridge
The bridge exercise strengthens the pelvic floor muscles and the glutes. In addition, it tightens the glutes while strengthening the core and alleviating back pain. The steps for this exercise are as follows:
- Lie on your back on the ground.
- Bend your knees and place your feet flat on the ground. Then, lift your hips a few centimeters off the ground.
- Hold this position for 10 seconds.
- As you lower yourself back down, relax the pelvic floor muscles and glutes.
- Rest for a few seconds, then repeat the exercise.
The exercise should be repeated at least 10 times. Over time, the number of repetitions should be increased.
Jump Rope
Some individuals experience stress incontinence, a type of urine leakage, during physical activities like jumping. This condition is caused by pressure on the bladder. Therefore, incontinence may occur during stressful situations like sneezing or coughing.
Jumping rope strengthens the pelvic floor. During the first few days or weeks of jumping rope, leakage may occur, but continuing the exercise will reduce and eventually stop the leakage.
Quick Contractions
This exercise is similar to Kegel exercises. However, in quick contractions, the pelvic muscles are rapidly contracted and relaxed. Therefore, during the exercise, the muscles should be quickly contracted and then immediately relaxed. This exercise should be performed in 10-20 repetitions, with breaks in between.
Overactive Bladder and Sexuality
The impact of overactive bladder on sexual health is not fully understood. However, overactive bladder generally has a negative impact on patients' lives. A cohort study comparing women with and without overactive bladder showed a significant decrease in sexual satisfaction in women with overactive bladder. Therefore, it is known that sexual satisfaction is lower in these women.
Incontinence during sexual intercourse occurs in 60% of women who experience this issue. This can be related to both stress incontinence and detrusor overactivity. However, incontinence during sexual intercourse is more common in those with stress incontinence. Additionally, urge incontinence due to urinary urgency also significantly affects the reduction in partner satisfaction.
Overactive Bladder Treatment and Sexuality
Research on overactive bladder and sexuality has largely focused on alleviating sexual dysfunction. Some studies examining the impact of the three stages of treatment for overactive bladder on sexuality have shown that these treatments increase sexual pleasure in women, while other studies show no significant increase. However, the common conclusion of the studies is that overactive bladder treatment does not have a negative impact on sexuality.
Overactive Bladder, Menopause, and Sexuality
Hormone therapy for menopausal women not only helps alleviate problems such as pain, orgasm issues, and lubrication but also reduces the severity of overactive bladder problems.
Both menopause and overactive bladder are significant contributors to sexual dysfunction. As age progresses, overactive bladder symptoms worsen, and because this coincides with the postmenopausal period, sexual dysfunctions are more common in women during this time. Therefore, both vaginal estrogen and overactive bladder treatment should be prescribed together for women in this period.
Behavioral Changes
Behavioral changes often used in treating overactive bladder may not help reduce the severity of the condition in some patients. However, changes such as reduced caffeine intake, bladder training, and weight loss can help alleviate sexual dysfunction.
Pelvic Floor Muscle Training
Exercises aimed at strengthening the muscles in the pelvic floor not only help alleviate overactive bladder symptoms but also address various pelvic floor disorders. In women with both overactive bladder and sexual dysfunction, performing pelvic exercises can alleviate symptoms and improve sexual issues.
A six-week study on this topic found a significant reduction in symptoms, excluding weight gain, in women with overactive bladder. Additionally, there was a notable increase in the Female Sexual Function Index. Therefore, patients should continue their exercises regularly to alleviate symptoms and enhance sexuality.
Medications Used in Overactive Bladder Treatment and Sexuality
Numerous studies have been conducted on the various drug groups used in treating overactive bladder. A significant portion of these studies has shown that the medications used in treatment significantly increase sexual arousal in women. Although anticholinergics are known to have a drying effect on mucosal tissue, they still show an increase in sexual arousal, albeit less so than other drug groups.
Neuromodulation and Sexuality
Neuromodulation, the final stage of overactive bladder treatment, involves tibial nerve or sacral nerve stimulation. While studies in this area are limited, the results obtained are promising.