30 Second Summary
- Overactive bladder is a disease characterized by the sudden need to urinate and urinary incontinence.
- It can occur in people of all ages, but is more common in women and the elderly.
- Causes include aging, caffeine, alcohol, stress and some medications.
- Lifestyle changes, medication, surgical intervention and other treatments can be applied.
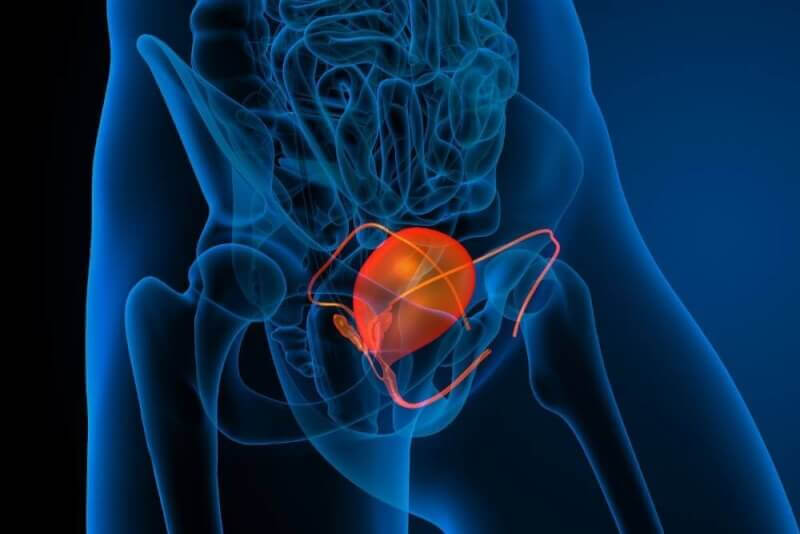
What is an overactive bladder?
Overactive bladder, also known as a nuisance bladder, refers to a number of problems that occur when patients feel an urgency to urinate. These problems do not include urine leakage or wetting accidents. Basically, patients with an overactive bladder refer to the frequent urge to urinate. It is a disease caused by the activity of the muscle group that allows the bladder to empty. For this reason, even if the bladder is not completely full, patients go to empty urine.
Symptoms of overactive bladder
Medically, the bladder should be emptied between 4 and 8 times a day. Patients who have more than eight urges to urinate are referred to as having an overactive bladder. The most common people are women of all age groups and the elderly.
Other symptoms of overactive bladder include wetting the bed, not being able to reach the toilet and going to the toilet more often at night. Leaking urine is not one of the symptoms of an overactive bladder. If patients experience this symptom, the problem is considered to be urinary incontinence due to urge incontinence.
Who has overactive bladder?
Overactive bladder is a common disease in all age groups and races. However, it is often seen in postmenopausal women and men with prostate disease. On the other hand, overactive bladder is often encountered in children who are just starting toilet training.
How is overactive bladder diagnosed?
The most important factor in the diagnosis of overactive bladder is the history of the patients. For this reason, patients are asked to keep a urine diary in order to diagnose overactive bladder. Information that should be specifically included in this diary includes the frequency of urination during the day and night, the comfortable intervals between trips to the toilet, the presence of sudden urgency, the ability to delay urination, the type of incontinence, whether pads are used, whether there is difficulty urinating, and the history of incontinence. In addition to this information, patients have a history of neurologic disease, vaginal or incontinence history and radiotherapy.
Causes of overactive bladder
It is possible to list the causes of overactive bladder as follows.
- Age-related erosion of cognitive skills
- Excessive consumption of alcohol, coffee and acidic drinks
- Diuretic drugs
- Conditions that prevent bladder emptying
- Hormone changes women experience during menopause
- Damage to the bladder muscles due to neurogenic diseases and treatments
- Diabetes
- Obesity
- Urinary tract infection
Overactive bladder treatment methods
There are many treatment options for overactive bladder. Determining the underlying causes of overactive bladder is important in deciding which treatment to choose.
Lifestyle changes
In the treatment of overactive bladder, patients are first asked to change their lifestyle if necessary. The first place among these changes should be the ideal weight of the patients. In addition, reducing caffeine intake, eliminating constipation by consuming plenty of fiber foods, reducing excessive fluid intake, reducing carbonated liquid intake, quitting smoking.
Pelvic floor muscle training
With pelvic floor muscle exercises, it is also possible to control the muscles that control the bladder. For this reason, Kegel exercises and biofeedback are applied to patients.
Behavior therapies
Another method used in the treatment of overactive bladder patients is behavioral training. This training is divided into three. Bladder training, timed voiding and habit training are among the trainings given to patients.
Electrical stimulation
Electrical stimulation, which is one of the treatments that should be applied every day, is one of the negative aspects of the treatment, as it covers at least 2 years of treatment. The pelvic floor muscles are electrically stimulated with probes inserted into the vagina.
Electromagnetic Therapy
Electromagnetic therapy is logically the same as electrical stimulation. However, this treatment method stimulates the pelvic muscles and sacral roots without a prop. Although the exact mechanism is not known, passive pelvic floor exercises control the overactivity of the muscles that control the bladder. The most negative aspect of the treatment is that it involves repeated sessions in a clinical setting.
Pharmacological treatment
Some medications are also used to control involuntary contractions of the muscles that control the bladder. The most commonly used drug group among these drugs is anticholinergic drugs. These drugs block the factors that cause stimulation of the bladder muscles. The first effects start to be seen within 2 weeks.
The effects and side effects of the medicines vary according to the patients. In patients with overactive bladder, urinary incontinence rates decrease by 70% to 75% and voiding frequency by 20% to 30%, while voiding volume increases by 10% to 20%.
In addition to these, there are also intra-bladder agent applications. Some of these agents are not yet available in our country. However, botulinum toxin, also known as Botox, is especially used in patients with treatment-resistant overactive bladder.
Sacral neuromodulation
With sacral neuromodulation, which has the highest cost among overactive bladder treatments, it is seen that 80% of patients have 50% of their storage symptoms resolved. The method of application is the insertion of the electrode at the sacral 3 level (S3) in the medulla spinalis. This electrode is continuously excited by the generator.
Augmentation cystoplasty
It is applied as the last option in the treatment of overactive bladder. It is used in patients who are refractory to treatment and as a last option for this treatment, but also in patients with severe symptoms. The aim of this procedure is to create a high functioning and low pressure bladder. In this procedure, the bladder of the patients is divided in two and a piece of intestine is added in between. In this way, the volume of the bladder is increased. It also acts as a buffer against involuntary contractions.