30-Second Summary
- Peritoneal dialysis is one of the treatment options that help remove waste products from the blood when the kidneys are not functioning properly.
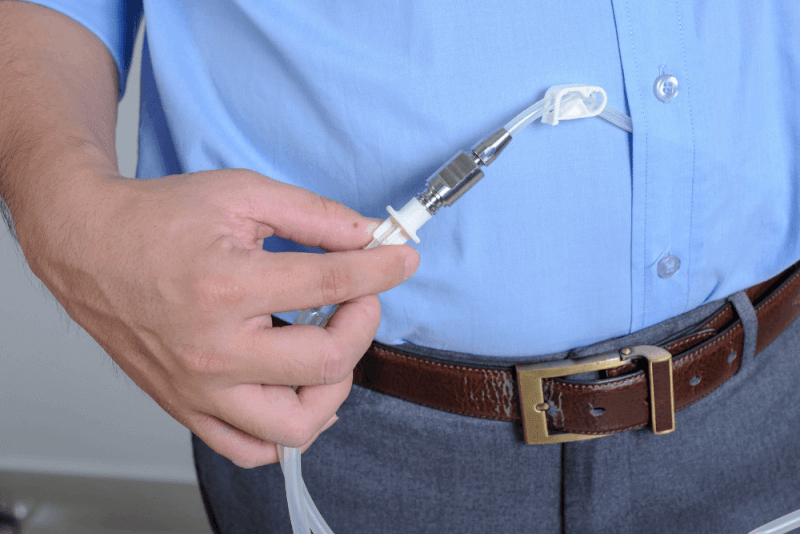
- During peritoneal dialysis, patients administer a cleansing solution into the abdominal area through a tube.
- The procedure of peritoneal dialysis is only possible after the surgical wound has healed. Patients must wait at least 2 weeks for this.
- Patients undergoing peritoneal dialysis must pay attention to their nutrition, as their kidneys are not capable of effectively removing waste and excess fluids from the body.
What is Peritoneal Dialysis?
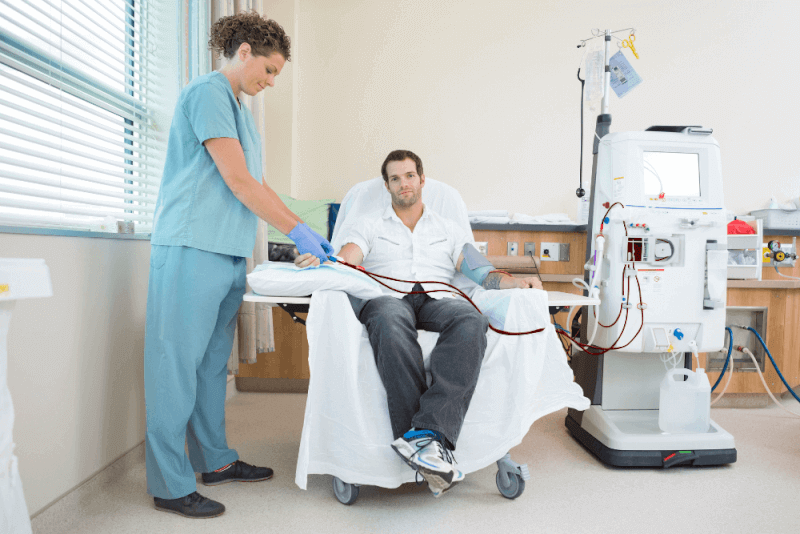
Peritoneal dialysis is a treatment option used to remove waste products from the blood when the kidneys cannot perform their function properly.
During peritoneal dialysis, patients administer a cleansing solution into their abdominal area through a tube. The abdominal lining, known as the peritoneum, acts as a filter, helping to clean the blood of waste products. After a certain period, the filtered waste-containing solution drains from the abdomen, and the blood is cleansed.
Unlike hemodialysis, which filters the blood outside the body, peritoneal dialysis works inside the body. Hemodialysis involves using an external machine to filter the blood.
Peritoneal dialysis can be done at home, at work, or while traveling. However, it is not suitable for all patients with kidney failure. To use this method, patients must be able to care for themselves and have manual dexterity.
Types of Peritoneal Dialysis
Peritoneal dialysis can be performed in two different ways. These types and their characteristics include the following:
Continuous Ambulatory Peritoneal Dialysis (CAPD)
This type of peritoneal dialysis does not require a machine. The process of administering and draining the cleansing solution, known as an exchange, is done during the patient's waking hours. The solution is introduced into the abdomen via a catheter. After the waiting period, gravity helps the solution drain out of the catheter.
In this method, patients need to perform 3-5 exchanges while awake. During sleep, exchanges with a longer waiting time are applied. The process can be done at home, on vacation, or at work. The important thing is to perform it in a clean and dry environment. During the waiting period, patients can continue their daily activities.
Automated Peritoneal Dialysis (APD)
Also known as Continuous Cyclic Peritoneal Dialysis, this method uses a machine called an automatic cycler. The machine automatically performs the exchange while the patient is asleep. While the patient sleeps, the machine fills the abdomen with the cleansing solution and ensures that it stays inside. After the waiting period, the machine automatically drains the solution.
During this method, patients must remain connected to the machine. A major advantage is that exchanges are not performed during the day, but in the morning, it may take longer to complete the drainage process.
What is Peritoneal Dialysis Used For?
Peritoneal dialysis is recommended when the kidneys are not functioning properly. Kidney damage typically worsens over time in the following conditions:
- Diabetes
- High blood pressure
- Glomerulonephritis, which causes damage to the kidneys' filtration system
- Genetic conditions like polycystic kidney disease, which causes multiple cysts in the kidneys
- Long-term use of painkillers like ibuprofen and naproxen, which can damage the kidneys
When the kidneys cannot adequately filter waste from the blood, peritoneal dialysis can be used to help remove the waste from the bloodstream and excrete it from the body.
Patients recommended for peritoneal dialysis typically have the following characteristics:
- The patient cannot cope with the side effects of hemodialysis
- A preference for a treatment that interferes less with daily routines
- Patients prefer easier work or travel options
- Some kidney function is still intact
However, peritoneal dialysis is not recommended in the following conditions:
- Previous surgery scars on the abdominal area
- Weakness in the abdominal muscles
- Patients unable to care for themselves or without sufficient support
- Diseases that affect the digestive system, such as inflammatory bowel disease
How is Peritoneal Dialysis Performed?
Before peritoneal dialysis can be performed, a preparation phase is required. During this phase, a catheter is inserted into the abdominal area to allow the cleansing solution to be introduced. This catheter is inserted through a short surgical procedure and is used to introduce the solution and expel the waste products.
The procedure of peritoneal dialysis can only be done after the surgical wound heals. Patients need to wait at least 2 weeks before starting the treatment. During this period, both the patients and their caregivers are trained in peritoneal dialysis techniques.
The Process of Peritoneal Dialysis
The steps involved in peritoneal dialysis include the following:
- The cleansing solution, called dialysate, is introduced into the abdomen via a catheter.
- The solution remains in the abdomen for 4-6 hours, known as the dwell time. The dwell time varies for each patient.
- The dextrose sugar in the dialysate helps filter waste products, chemicals, and extra fluid from the blood, which are filtered by small blood vessels in the peritoneum.
- At the end of the dwell time, the solution and waste products are drained out through the catheter.
The application method varies depending on the type of peritoneal dialysis. If continuous ambulatory peritoneal dialysis (CAPD) is used, these steps are performed manually during the patient’s waking hours. If automated peritoneal dialysis (APD) is used, the process is carried out automatically by a machine during the patient's sleep.
Peritoneal Dialysis and Nutrition
Patients undergoing peritoneal dialysis need to pay attention to their nutrition, as their kidneys cannot effectively remove waste and excess fluids from the body. It is important to have the right amount of protein, calories, vitamins, and minerals in the diet. Patients are advised to prepare a nutrition plan in collaboration with a dietitian to maintain a balanced diet.
Importance of Catheter Cleaning in Peritoneal Dialysis
Patients undergoing peritoneal dialysis are at a higher risk of infections. Therefore, special care must be taken with the catheter area, and in-depth information should be gathered on how to properly clean it. Additionally, attention should be given to the following points:
- Wash hands with warm water and soap before touching the catheter.
- The catheter area should be cleaned daily. It is important to consult a doctor about which cleaning solution to use for this purpose.
- The catheter should be kept clean and dry, except during showering.
- During exchanges, surgical masks and gloves should be worn.
Risks of Peritoneal Dialysis
Complications that may occur in patients undergoing peritoneal dialysis include:
Infections
Peritonitis, which is an infection of the peritoneum, is a common complication of peritoneal dialysis. Infections can also start at the catheter insertion site. If the person performing the dialysis is not adequately trained, the risk of infection increases.
Weight Gain
The dialysis fluid contains a sugar called dextrose. If the body absorbs some of this fluid, it can lead to an intake of several hundred extra calories per day, which may result in weight gain. This can also lead to elevated blood sugar levels and cause diabetes.
Hernia
Long-term retention of fluid in the abdomen can cause strain on the abdominal muscles and potentially lead to a hernia.
Reduced Effectiveness of Treatment
After a few years, peritoneal dialysis may become less effective, and patients may need to be referred to hemodialysis or a kidney transplant.
Things to Consider in Peritoneal Dialysis Treatment
Patients who are undergoing peritoneal dialysis should keep the following in mind:
- Avoid medications that can damage the kidneys, including non-steroidal anti-inflammatory drugs (NSAIDs).
- Do not take baths in the tub.
- Avoid swimming in pools without chlorine or lakes.
- Once the catheter surgery site has healed, patients can swim in pools or the sea, but after swimming, they should ensure the area is kept dry by wearing dry clothes.
Outcomes of Peritoneal Dialysis Treatment
The goal of peritoneal dialysis is to remove waste and excess fluid from the blood effectively. Several factors affect how well the treatment works, including:
- The patient's overall health condition
- How quickly the peritoneum filters waste
- The type of dialysis solution used
- The number of exchanges done daily
- The dwell time
- The concentration of sugar in the dialysis solution
To check if the dialysis is removing enough waste, regular tests should be done on the patients. These tests include:
Peritoneal Equilibration Test (PET)
This test compares samples of blood and dialysis solution during the exchange. The results show how quickly waste toxins pass from the blood into the dialysis solution. This helps determine the optimal dwell time for effective filtration.
Clearance Test
In this test, blood and used dialysis fluid are checked for urea levels. The test helps determine how much urea is removed from the blood during dialysis. If the body is still producing urine, the amount of urea in the urine is also checked.
If test results indicate that the dialysis routine is not removing enough waste, doctors may recommend the following adjustments:
- Increasing the number of exchanges
- Increasing the volume of dialysis solution used in each exchange
- Using a dialysis solution with a higher concentration of dextrose