Also known as thalassemia, Mediterranean anemia is a type of anemia that is genetic and prevalent in the Mediterranean region. In our country, there are about 1.4 million carriers of Mediterranean anemia, and approximately 4,500 affected individuals.
Among the most common genetic disorders in our country, Mediterranean anemia occurs in children at a rate of 25% if either parent is a carrier. Thalassemia can be detected through screening tests and thus is preventable.
What is Mediterranean Anemia?
It is a disease characterized by a genetic deficiency in the synthesis of the beta globin chain of hemoglobin, the substance that gives blood its red color. In severe thalassemia, known as thalassemia major, patients require regular blood transfusions. For less severe cases, it is called thalassemia minor. The clinical presentation of patients can vary between these two severities, referred to as thalassemia intermedia.
In children where both parents are carriers, the type of anemia seen is homozygous, or thalassemia major, whereas if only one parent is a carrier, the children will have heterozygous, or thalassemia minor.
Thalassemia is generally found in countries around the Mediterranean, but also in regions in Africa and South Asia. These regions also frequently experience malaria, which is thought to correlate with the disease.
Mediterranean Anemia Carrier
Being a carrier of thalassemia means carrying one of the genes responsible for this disease. However, carriers, also known as minor thalassemia, do not show symptoms of Mediterranean anemia and never develop the full disease, although they may sometimes show mild anemia symptoms. The symptoms, characterized by red blood cells being smaller than normal, do not require treatment.
Anyone can be a carrier of thalassemia, though it is more common among certain ethnic groups. These groups include:
- Countries around the Mediterranean including Greece, Italy, and Cyprus
- India, Pakistan, and Bangladesh
- The Middle East
- China
- Southeast Asia
Carrier Symptoms of Mediterranean Anemia
Carriers of Mediterranean anemia never develop the disease; therefore, they typically do not exhibit any symptoms. However, it has been observed that some carriers have red blood cells that are smaller than standard. This condition may lead to mild anemia, which does not require treatment.
Causes of Mediterranean Anemia
Mediterranean anemia is a genetic disease caused by gene mutations. Research on thalassemia patients has identified over 200 gene mutations, which result in insufficient synthesis of the globin protein of hemoglobin. This disrupts hemoglobin synthesis.
Who Gets Mediterranean Anemia?
The sole reason for the occurrence of Mediterranean anemia is a family history of the disease.
Is Mediterranean Anemia Fatal?
Mediterranean anemia causes a disruption in the structure of red blood cells that carry oxygen in the blood. As a result, these malformed cells die, leading to varying degrees of anemia in patients. Severe anemia can lead to irregular heartbeat, heart failure, organ damage due to oxygen deficiency, and respiratory problems. If not treated, these complications associated with thalassemia can be fatal.
Symptoms of Mediterranean Anemia
The division of Mediterranean anemia into three different groups also leads to a diversification of symptoms in patients.
Symptoms of Thalassemia Major
Thalassemia major, the most severe type of Mediterranean anemia, typically shows its first symptoms at around six months of age. Symptoms seen in infants and children include:
- Concentration problems,
- Bone pain, particularly in the legs and other bones,
- Symptoms related to iron accumulation due to repeated blood transfusions,
- Prominent facial bones,
- Heart failure,
- Palpitations,
- Enlargement of the heart
- Abdominal swelling due to enlargement of the liver and spleen,
- Jaundice,
- Frequent infections,
- Growth retardation,
- Lack of appetite,
- Paleness,
Symptoms of Thalassemia Minor
Thalassemia minor, the mildest form of Mediterranean anemia, shows symptoms of mild anemia and iron deficiency.
Symptoms of Thalassemia Intermedia
Symptoms found in this moderately severe form of anemia include:
- Enlargement of the spleen,
- Weak bones,
- Growth and developmental retardation,
- Excessive fatigue,
- Paleness,
How is Mediterranean Anemia Diagnosed?
Mediterranean anemia is usually diagnosed in children between the ages of 6 and 12 years, but if it is thalassemia major, symptoms can start from infancy. The tests conducted for diagnosis include:
- Complete blood count, which measures the size and number of different blood cells in a given volume of blood,
- Hemoglobin electrophoresis test, which measures HbA and HbA2 levels (in thalassemia patients, the HbA value is low while the HbA2 value is high. In pregnant patients, this test is performed using a sample from cord blood.),
- Serum iron and iron binding capacity levels.
Treatment of Mediterranean Anemia
The treatment approaches for Mediterranean anemia depend on the severity of the disease. While no treatment is needed for thalassemia minor and intermedia, the following treatments are administered to patients with thalassemia major:
- Administration of pneumococcal, meningococcal, hepatitis, and Haemophilus influenzae type B vaccines,
- Avoidance of iron-containing medications,
- Bone marrow transplant,
- Regular monitoring of heart and lungs,
- Removal of the gallbladder,
- Daily supplementation with folic acid,
- Splenectomy if necessary,
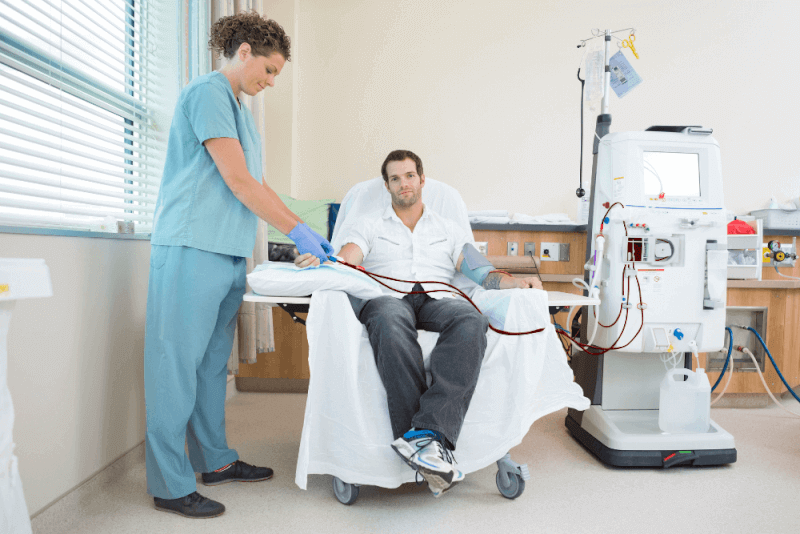
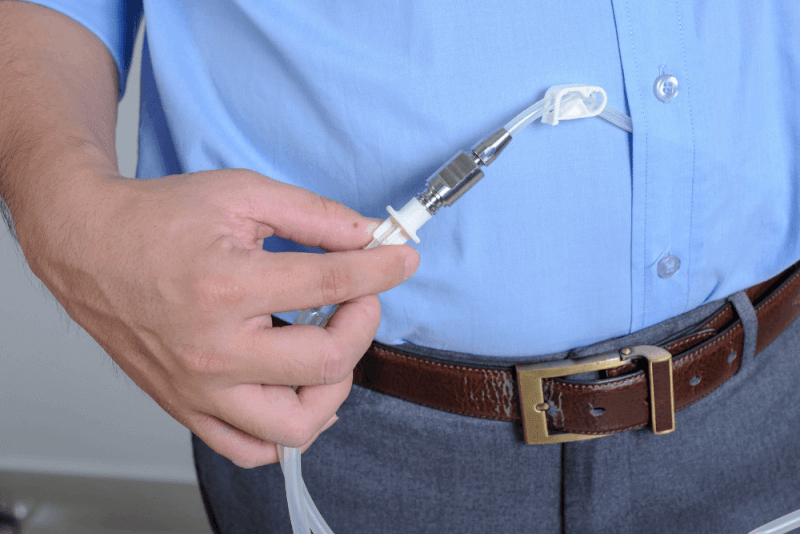
- Regular blood transfusions,
- Medications to prevent iron accumulation.
Risks of Mediterranean Anemia
Many health issues caused by Mediterranean anemia can be managed with appropriate treatments. However, it is a serious health condition that can significantly impact patients' lives.
Even in mild cases, there is a risk of passing a severe form of the disease to children. Therefore, if the disease is not closely monitored, it can lead to severe organ damage and pose a threat to life.
Thanks to improvements in treatments, patients with Mediterranean anemia can now live beyond the age of 60. However, regular treatment is necessary for a long life. Otherwise, patients may face early death.
Complications of Mediterranean Anemia
The complications of Mediterranean anemia vary with the severity of the disease.
Thalassemia Minor
Patients with thalassemia minor are also carriers of Mediterranean anemia. It is advised that these individuals do not marry others carrying the same disease.
Thalassemia Intermedia
In patients with thalassemia intermedia, complications vary based on the severity of the disease and include stunted growth, enlarged spleen, and weakened bones.
Thalassemia Major
Patients with beta thalassemia major experience significant complications, including a higher likelihood of early mortality. Complications of major thalassemia include bone issues causing facial changes, delayed growth, gallbladder and liver problems, enlarged kidneys, enlarged spleen, hypothyroidism, diabetes, and heart problems.
Due to the frequent blood transfusions required by thalassemia major patients, iron may accumulate in tissues. Excess iron in the body adversely affects the heart, hormone-producing glands, endocrine system, and liver.
Patients who have had their spleen removed are particularly prone to infections.
Thalassemia major causes the expansion of bone marrow, which, in turn, leads to bone widening. This results in bones that are more fragile and thin, and it can also cause shape changes in the skull, especially.
The excessive destruction of red blood cells in thalassemia patients necessitates that the spleen works harder, leading to its enlargement, which can worsen anemia. Therefore, splenectomy is often recommended.
Risk Factors for Pregnant Women with Mediterranean Anemia
- Low bone density,
- Increased need for blood transfusions,
- Hypothyroidism,
- Low thyroid levels,
- Heart issues,
- Gestational diabetes,
- Higher risk of infection,
Mediterranean Anemia and Marriage
There is no restriction on marriage for people with Mediterranean anemia as thalassemia is a genetic disease and not contagious. However, IVF is generally recommended for patients wishing to have children due to the risk of genetic transmission. The chances of passing genes to children are as follows:
- If a person with Mediterranean anemia marries a healthy person, there is a 50% chance that the children will be carriers.
- If two people with Mediterranean anemia marry, there is a 100% chance that the children will have the disease.
- If a person with Mediterranean anemia marries a carrier, the children have a 50% chance of having the disease and a 50% chance of being carriers.
If a carrier marries another carrier, the children have a 50% chance of being carriers, a 25% chance of being healthy, and a 25% chance of having the disease.
Mediterranean Anemia and Nutrition
Nutrition plays a crucial role in the management of Mediterranean anemia. The foods that patients should consume or avoid are directly related to the treatment they are undergoing. Here are some dietary considerations for thalassemia patients:
Foods to Avoid
There are certain foods that patients with Mediterranean anemia should exclude from their diet, as these can exacerbate the complications associated with the disease.
Iron
Iron is necessary for hemoglobin production, which binds and transports oxygen within red blood cells. Iron is also required for many enzymatic reactions and plays a key role in the immune system.
Patients receiving regular blood transfusions for Mediterranean anemia often experience iron accumulation. Even some non-transfused patients may absorb excessive iron from the intestines. This iron accumulation can damage organs such as the spleen, liver, and heart.
Therefore, patients with high iron levels are advised to consume foods low in iron. Additionally, foods high in vitamin C, which enhances iron absorption, should be limited.
There are two forms of iron: animal-based, found in red meat and dairy products, and plant-based, especially in leafy greens, which are rich in iron. Plant-based iron dissolves and metabolizes faster.
In a low-iron diet, patients may consume small amounts of meat, fish, or foods rich in vitamin C, as well as whole grains and root vegetables. A moderate iron diet includes whole grains, root vegetables, and some vitamin C-rich foods and red meat, while an iron-rich diet includes ample amounts of meat, poultry, and fish.
One essential point is that non-transfused patients should not entirely eliminate iron-rich foods from their diet, as these foods also contain important minerals like zinc.
For patients following an iron-restricted diet, here are some recommended additions:
- Calcium-rich dairy products, as they reduce iron absorption.
- Tea, which contains tannins that decrease iron absorption.
- Whole grains, wheat bran, corn, oats, rice, and soy, which reduce the amount of iron absorbed and counteract the effect of vitamin C.
- Dark chocolate, peanut butter, hemp seeds, and artichokes, which are high in iron and should be used sparingly in the diet.
Individuals with Mediterranean anemia should avoid iron supplements, and they should carefully check the contents of multivitamins and other supplements.
Foods to Consume
There are specific foods that Mediterranean anemia patients should include in their diets, as these foods help protect against the adverse effects of the disease.
Calcium
Calcium sources are essential for bone development and managing the disease. Calcium strengthens bones by supporting their durability and structure, with bones serving as storage sites for calcium to be used by the body.
Calcium also reduces iron absorption, so dairy products are often recommended with meals. Osteoporosis is commonly seen in Mediterranean anemia patients, and to prevent this, calcium should be consumed with vitamin D, as it aids calcium absorption in the body.
Foods rich in calcium include:
- Milk and dairy products
- Bread enriched with calcium
- Certain leafy green vegetables like broccoli and cabbage (although spinach is rich in calcium, it is also high in iron and should be consumed in moderation)
- Fortified soy products
- Fish that can be eaten with bones, like sardines
Zinc
Zinc, unlike iron, cannot be stored in the body and thus needs to be consumed daily. Key functions of zinc in the body include:
- Optimal immune function
- Optimal growth
- Bone health
- Bone density
- Pubertal development
- Glucose homeostasis, beneficial for individuals with diabetes
Studies on Mediterranean anemia patients indicate that a significant number have zinc deficiency, especially those receiving blood transfusions. Therefore, zinc-rich foods should be added to their diets, but since zinc can affect the absorption of certain nutrients, patients should consult a doctor before adding these foods.
Foods rich in zinc include:
- Red meat, the most important source of zinc
- Chicken
- Pumpkin seeds
- Peas
- Milk and dairy products
- Eggs
- Shellfish
- Whole-grain cereals
- Nuts
- Legumes
Zinc in nuts and legumes may be limited by phytates present in these foods, so it is recommended to soak legumes before consumption.
Vitamin E
While oxygen is essential for life, it can sometimes convert into chemical substances called free radicals in the body. Under controlled conditions, free radicals have important uses, but uncontrolled reactions can cause significant damage and disease.
Antioxidants are crucial in any diet, as they help control free radicals and prevent oxidative damage. They also play a role in preventing diseases like coronary heart disease and cancer. Due to iron accumulation, Mediterranean anemia patients are at higher risk of oxidative damage.
Vitamin E, an important antioxidant, supports immune function. Foods rich in vitamin E include:
- Olive oil, one of the best sources of vitamin E, which also protects against heart disease. Olive oil should be consumed raw as heat can reduce its vitamin E content.
- Wheat germ oil
- Sunflower seeds
- Almonds
- Sunflower oil
- Safflower oil
- Hazelnuts
- Peanut butter
- Corn oil
- Spinach
- Broccoli
- Soybean oil
- Kiwi
- Mango
- Tomatoes
Foods to Consume in Limited Quantities
There are some foods that Mediterranean anemia patients should include in their diet but consume in limited amounts. While these foods can help manage the disease, excessive intake may be harmful.
Foods that should be consumed in limited quantities include:
- Red meat, grains, liver, oysters, pork, beans, peanut butter, and tofu due to their high iron content and their ability to enhance iron absorption
- Fruit juices, fruits, and vegetables rich in vitamin C, which increase iron absorption
- Fermented foods like sauerkraut, pickled onions, turnips, carrots, fermented soy products, and alcohol, which enhance iron absorption
- Iron-fortified foods like flour tortillas, infant cereals, creamed wheat, and breakfast cereals due to their iron content and iron absorption enhancement
Healthy Food Substitutions
It can be challenging for patients to change their diet all at once. Therefore, they can replace foods that should be removed from their diet with healthier alternatives. Some suggested substitutions include:
- Replace ground beef with ground turkey
- Replace vitamin C-rich fruits with options like cherries, apples, plums, and apricots
- Replace vitamin C-rich vegetables with options like mushrooms, cucumbers, celery, and beets
- Replace fatty parts of chicken, such as the thigh, with leaner parts like the breast
- Replace alcohol with non-alcoholic cocktails and diet sodas
- Replace full-fat dairy products with low-fat options
- Replace fruit juices with squash juice
- Replace grains with oats
Easy Tips for Daily Routine
Even small changes in the daily routine of Mediterranean anemia patients can make a significant difference in managing the disease. Here are some helpful tips:
- Drinking tea after a meal rich in iron and vitamin C can reduce iron absorption. However, it is recommended to drink coffee only once a day as it may contribute to osteoporosis.
- Adding dairy products to meals
- Getting 20 minutes of sunlight each day
- Adding turmeric to meals