What is Lung Thickening (Pulmonary Fibrosis)?
Pulmonary fibrosis is a lung disease that occurs when lung tissue is injured or damaged, making it difficult for the lungs to function properly. While this disease tends to worsen over time, it is possible for some individuals to remain stable for a long period. However, this is uncommon. Patients generally deteriorate quickly, with worsening shortness of breath.
The scarring in the lungs can be caused by many different factors. Often, experts cannot determine the exact cause of the injury. This condition is called idiopathic pulmonary fibrosis.
Idiopathic pulmonary fibrosis usually occurs in middle-aged and older adults. Although it can also be seen in infants and children, it is not very common.
The lung damage caused by pulmonary fibrosis cannot be repaired. However, medications and therapies can help slow the progression of the disease and alleviate symptoms. Lung transplantation is one of the treatment options for this disease.
Diagnosis Methods for Lung Thickening (Pulmonary Fibrosis)
During the diagnosis of pulmonary fibrosis, the patient's medical history is first reviewed. Additionally, a physical examination is conducted to carefully evaluate the symptoms. During the physical examination, a stethoscope may be used to listen to the lungs and check for abnormal sounds. Diagnosing pulmonary fibrosis can be challenging because its symptoms can resemble those of other common lung diseases. Therefore, one or more tests may be required to confirm the diagnosis.
Blood Tests
Experts may order various blood tests to rule out other diseases or determine the causes of symptoms. Laboratory tests also help experts monitor the progression of the disease after diagnosis.
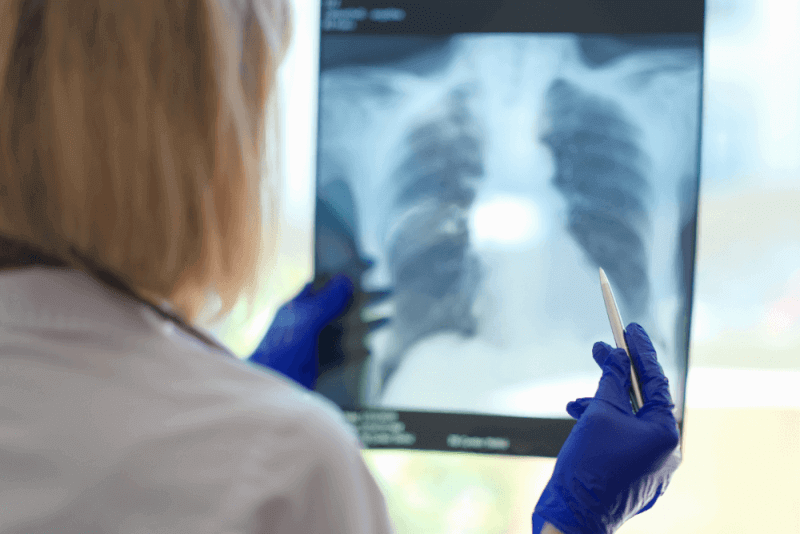
Imaging Tests
Chest X-rays or CT scans can help rule out lung-related diseases. These images are useful for confirming the diagnosis of pulmonary fibrosis, as they can clearly show the scarring in the lungs.
Breathing Tests
Pulmonary function tests, also known as breathing tests, measure lung function and capacity using different devices. Breathing tests include the following:
Spirometry
In this test, you exhale quickly and forcefully through a tube connected to a machine. The machine measures how much air the lungs can hold and how quickly air can move in and out of the lungs.
Lung Volume Test
This test measures the amount of air the lungs hold at different times during breathing.
Lung Diffusion Test
This test shows how well the body transfers oxygen and carbon dioxide between the lungs and the blood.
Pulse Oximetry
This simple test uses a small device placed on one of the fingers to measure the amount of oxygen in the blood. The percentage of oxygen in the blood is called oxygen saturation.
Exercise Stress Test
An exercise test performed on a treadmill or stationary bike can be used to monitor heart and lung function during activity.
Arterial Blood Gas Test
In this test, a blood sample is usually taken from an artery in the wrist. The levels of oxygen and carbon dioxide in the sample are measured.
Oxygen Desaturation Study
This test measures the oxygen level in the blood. A probe is placed on the finger or forehead, and the patient walks for 6 minutes while oxygen levels are measured.
Biopsy
Biopsy involves removing a small sample of lung tissue through a small incision in the ribs. The sample is then examined in a laboratory setting.
Symptoms of Lung Thickening (Pulmonary Fibrosis)
Pulmonary fibrosis does not affect everyone in the same way. It can cause symptoms similar to many common and easily treatable health conditions. Sometimes, these symptoms can resemble those of a cold or upper respiratory infection.
Common symptoms of pulmonary fibrosis include:
- Shortness of breath with shallow, rapid breathing
- Persistent dry cough
- Unintentional and unexplained weight loss
- Shortness of breath, especially during or immediately after exercise
- Fatigue
As the disease progresses, additional symptoms may include:
- Changes in the appearance of the fingertips or toes
- Bluish skin or gray or white skin around the eyes or mouth due to low oxygen levels in the blood
Additionally, patients may experience difficulty breathing due to the scarring in their lungs. Despite their efforts, they may feel like they cannot breathe or take deep breaths.
Causes of Lung Thickening (Pulmonary Fibrosis)
Many different factors, such as smoking, can cause pulmonary fibrosis. The cause of a significant number of cases is unknown. Some types of pulmonary fibrosis can run in families. However, the groups at higher risk of developing pulmonary fibrosis include:
- Most patients are between 50 and 70 years old.
- Pulmonary fibrosis is more common in men.
- Smoking increases the risk.
- Regular exposure to chemicals or hazardous substances can damage the lungs. For this reason, hairdressers, farmers, stone cutters, or metal workers are at high risk.
- Certain health conditions, such as autoimmune diseases and viral infections, can also cause pulmonary fibrosis.
- Cancer treatments such as chemotherapy and radiation therapy can damage lung tissue.
- Certain medications, such as amiodarone used to treat irregular heartbeats, can damage lung tissue.
- Some types of antibiotics, such as nitrofurantoin or ethambutol, can also cause lung damage.
- Some anti-inflammatory drugs can cause lung damage, leading to pulmonary fibrosis.
- Lupus
- Dermatomyositis
- Mixed connective tissue disease
- Pneumonia
- Polymyositis
- Sarcoidosis
- Scleroderma
Treatment Methods for Lung Thickening (Pulmonary Fibrosis)
The scarring and thickening of the lungs caused by pulmonary fibrosis cannot be repaired. Moreover, no existing treatment can stop or reverse the progression of the disease over time.
However, some treatments can temporarily improve symptoms or slow the disease's progression. Additionally, certain treatments can help improve the quality of life. The treatment for pulmonary fibrosis varies depending on the cause. The severity of the condition is also important in treatment planning.
Medication Therapy
Medications such as pirfenidone or nintedanib may be recommended for individuals with idiopathic pulmonary fibrosis. These drugs are FDA-approved for the treatment of idiopathic pulmonary fibrosis. Nintedanib is also used for other rapidly progressing types of pulmonary fibrosis. These medications help slow the worsening of the disease and can prevent sudden flare-ups of symptoms.
Nintedanib can cause side effects such as diarrhea and nausea. Side effects of pirfenidone include nausea, loss of appetite, and skin rashes caused by sunlight. If either drug is prescribed, experts will regularly perform blood tests to monitor liver function.
If patients have GERD symptoms, acid-suppressing medications are also prescribed. GERD is a common issue, particularly in individuals with idiopathic pulmonary fibrosis.
Oxygen Therapy
The use of supplemental oxygen, also known as extra oxygen, cannot stop lung damage. However, it is effective in the following situations:
- Eases breathing and exercise
- Prevents or reduces complications caused by low blood oxygen levels
- Reduces stress on the right side of the heart
- Improves sleep
Pulmonary Rehabilitation
Pulmonary rehabilitation helps manage symptoms and improve the ability to perform daily tasks. Pulmonary rehabilitation programs focus on the following:
- Breathing techniques to help the lungs use oxygen more efficiently
- Emotional counseling and support
- Nutritional counseling
- Physical exercise
- Education about the condition
Sudden Worsening of Symptoms
In cases of sudden worsening of symptoms, also known as acute exacerbation, patients may need additional oxygen support. In some cases, mechanical ventilation in a hospital may be required. This treatment involves directing a tube into the lungs and connecting it to a machine that helps with breathing. When symptoms suddenly worsen, healthcare providers may recommend antibiotics, steroids, or other medications.
Lung Transplantation
Lung transplantation may be an option for some patients with pulmonary fibrosis. A lung transplant can improve the quality of life and allow for a longer life. However, lung transplantation comes with complications, such as rejection and infection. After a lung transplant, patients will need to continue taking medication for the rest of their lives.
Complications of Pulmonary Fibrosis
Complications caused by pulmonary fibrosis include:
High Blood Pressure in the Lungs
This type of high blood pressure, also known as pulmonary hypertension, affects the arteries in the lungs, called pulmonary arteries. Stiff and thick arteries can slow or block blood flow in the lungs. This increases the pressure inside the pulmonary artery and the right lower heart chamber called the right ventricle.
Right-Sided Heart Failure
This very serious condition occurs when the right chamber of the heart has to pump harder than usual to move blood through partially blocked arteries.
Respiratory Failure
Respiratory failure is usually the final stage of long-term lung disease. It occurs when the oxygen level in the blood drops to dangerously low levels.
Lung Cancer
Long-term pulmonary fibrosis increases the risk of developing lung cancer.
Other Lung Problems
The long-term worsening of pulmonary fibrosis can lead to serious issues such as blood clots in the lungs, lung collapse, or lung infection.